A partnership between Cancer Research UK and Blood Cancer UK has resulted in the UK’s leading biomedical research resource dedicated to storing samples and data of cancers in children and young people. What will this mean for the cancer research community? We spoke to Professor Christina Halsey to find out…
The VIVO Biobank provides a single point of access for people and organisations involved in researching blood, bone marrow and solid cancers in the young. By merging two existing biobanks – the Children’s Cancer and Leukaemia Group Tissue Bank and Blood Cancer UK’s CellBank – the partnership has created the widest collection of youth cancer samples available, helping to advance the high-quality research needed to develop new treatments faster.
But how, exactly, can it do that? We spoke to Professor Christina Halsey, paediatric oncologist and Head of the School of Cancer Sciences at the University of Glasgow to get some answers.
Collaboration seems particularly key in paediatric cancer research… do you think assets like biobanks can catalyse collaborative working?
Absolutely, when patients generously donate samples for biobanking they expect that they will be used for the common good – and maximising the scientific value of every sample is key to this.
We have always been fortunate in childhood cancer that our biobank samples often have really high-quality linked patient and trial data – allowing us to select samples on the basis of disease subtype or patient outcome. We are now moving a step further and feeding back to the biobank any work done on samples such as RNA-sequencing or proteomics etc. This means that other researchers, requesting samples from the same patient or cohort, can be put in touch with those who have already worked on these samples. This immediately forges collaborations as well as making obvious economic and scientific sense.
There are some very specific challenges that research into childhood cancer must address… what are these, and do you think they have been somewhat neglected?
Indeed! Childhood cancers are thankfully rare diseases – although their contribution to biological understanding of fundamental cancer biology and insights into how to achieve therapeutic success punch way above their weight.
The small numbers are further compounded by our recognition of the genetic and biological heterogeneity even within one subtype of cancer – meaning that sometimes we are getting down to single figures for patients with a particular cancer subtype in the UK. Single figure patient numbers are never going to be attractive to industrial partners making innovation and pharma partnerships particularly challenging in this space. It also means that fewer researchers are funded to work in this field and collaborative research partnerships are commonly international rather than national. This international working is a real bonus when it comes to diversity of thinking but really challenging when considering sharing data across borders, funding models and even simple things like sample sharing and courier costs!
“Predicting and preventing acute side-effects and longer-term toxicity is likely to be an emerging area of research over the next decade”
Another huge challenge is the need to consider long-term outcomes as well as short-term cure when treating our young patients whose normal tissues and organs are still growing and developing. We cure over 90% of children with leukaemia, and with a peak age of 2-5 years old at diagnosis that means they might hope for 80 or 90 years of healthy life ahead of them. The impact of our intensive chemotherapy regimens on the brain, heart, bones and pretty much every organ is considerable – and can result in long-term ill-health and a high incidence of second-cancers later in life. This is not only heart-breaking for the individual and family but also has profound socioeconomic and societal impacts.
Cancer research to date has had a very strong focus on novel treatments and has neglected toxicity. With a new focus on early detection and potentially picking up cancers that previously peaked in people in their 70s onwards in younger and younger populations I think patients will demand to know the long-term impact of any early interventions. Thus, predicting and preventing acute side-effects and longer-term toxicity is likely to be an emerging area of research over the next decade.
Your own work focusses on specific side-effects of current treatment for childhood leukaemia – tell us a little about that…
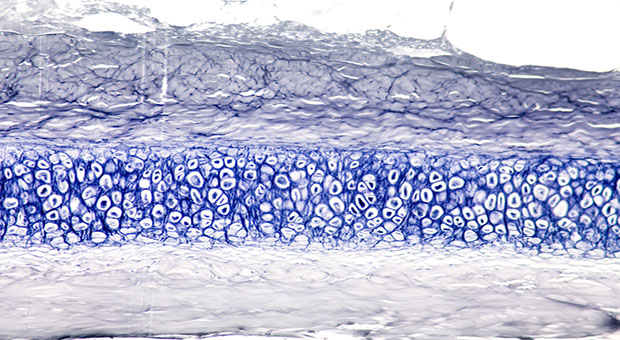
As I say, childhood leukaemia survivors often have lasting morbidity from the impact of chemotherapy on developing organs. The brain is particularly vulnerable; 20-40% of childhood acute lymphoblastic leukaemia (ALL) survivors have neurocognitive deficits secondary to use of universal, aggressive central nervous system (CNS) directed therapy. Treatment involves up to 26 lumbar punctures, often under general anaesthesia, to deliver intrathecal therapy. Despite this burdensome and toxic therapy, there have been no new drugs licensed for CNS-ALL since the 1960s, when very limited anti-leukaemic agents were available and there was no knowledge of molecular mechanisms of CNS leukaemia.
My research aims to understand the biology of CNS-leukaemia to develop low-toxicity CNS-directed therapy. A second focus of my group is to understand more about the risk-factors and mechanisms of neurotoxicity in order to develop novel interventions to prevent, ameliorate or detect neurotoxicity as it emerges.
How has this work benefitted from biobanking?
The Childhood leukaemia CellBank has built up collection of cerebrospinal fluid samples from children undergoing treatment for ALL, alongside clinical outcome data indicating which children have relapsed in the CNS or suffered neurotoxic adverse events. There is also matched DNA and live cells with which we can generate patient derived xenografts. This rich resource has benefited my work on multiple fronts. We have been able to use live cells to show that ALL cells, regardless of genetic subtype, possess an intrinsic ability to enter the CNS, and that relapse is determined by the ability to survive in this compartment rather than the ability to get there in the first place. This has important implications for treatment and risk-stratification. We have also used CSF samples to investigate protein, cfDNA and metabolic biomarkers that might be able to guide risk adapted therapy. Finally, we are currently undertaking a deep phenotyping/genotyping effort using DNA from the bank to investigate genetic susceptibility to adverse neurocognitive outcomes.
Looking at the wider picture of cancer research generally… how impactful has the development of biobanking been?
I think biobanking has had an enormous impact. The use of patient samples has opened our eyes to genetic heterogeneity within and between patients and allowed us to test new treatments against panels of cells/tissue samples that represent the true spectrum of clinical disease. It has driven the development of high-fidelity preclinical models and meaningful physiologically relevant drug screening. With new advents in multi-omic profiling of samples and artificial intelligence the benefits to patient centred research will continue to grow and grow.
As the CCLG Tissue Bank and Cellbank come together, what is the significance, as you see it, for a merged biobank for cancer researchers?
This has been a fantastic initiative, leukaemia research is much closer to solid tumours than we think – and the opportunities for shared learning, knowledge exchange and developing a critical mass within the UK to leverage the power of data and sample driven science are enormous. We already work together on many shared initiatives such as SMPaeds and have several basket trials open to solid tumour and leukaemia patients with shared driver mutations so the merging of our tissue banks is a logical extension to this breaking down of boundaries between our sister fields.
Childhood cancer researchers have always excelled at ‘team science’ so I am confident that this will lead to great synergy and accelerated progress for the benefit of our patients.
VIVO Biobank is creating a single research resource for accessing samples of cancers in children and young people. Building on the samples previously collected by the CCLG Tissue Bank and CellBank, the network provides access to the widest collection of historic, current, and future samples and data available.
 Professor Christina Halsey is Professor of Paediatric Haemato-Oncology & Head of the School of Cancer Sciences at the University of Glasgow. She is also an Honorary Consultant Paediatric Haematologist at the Royal Hospital for Children in Glasgow.
Professor Christina Halsey is Professor of Paediatric Haemato-Oncology & Head of the School of Cancer Sciences at the University of Glasgow. She is also an Honorary Consultant Paediatric Haematologist at the Royal Hospital for Children in Glasgow.