, by Elia Ben-Ari
A new type of targeted immunotherapy drug shrank tumors in about one in three people with small cell lung cancer (SCLC), the most aggressive form of lung cancer, according to results from a clinical trial. The findings are encouraging because little progress has been made in treating advanced SCLC, experts said.
Many people with SCLC respond to initial treatment with chemotherapy and immunotherapy. But the cancer usually progresses despite additional treatment, with most of these patients dying within weeks or months.
The early-stage clinical trial tested two different doses of an experimental drug called tarlatamab in people with SCLC whose cancer had progressed after at least two previous types of treatment. Many people in the study had already received at least three different treatments.
In the trial, tumors shrank in 40% of people given 10 mg of tarlatamab every 2 weeks and in about 32% of people who received a 100 mg dose.
Furthermore, in more than half of all patients whose tumors shrank with tarlatamab, the treatment kept the cancer at bay for at least 6 months—and in many, it did so for 9 months or longer.
This last finding was especially noteworthy, said Anish Thomas, M.D., of NCI’s Center for Cancer Research, who studies SCLC but was not involved in the trial.
“This is probably one of the most promising treatments being tested in small cell lung cancer right now,” Dr. Thomas said. The new findings are “hopeful for patients and the people who treat them, especially since this is such an aggressive disease with very few advances in treatment since the 1980s,” he continued.
Results of the trial—known as DeLLphi-301 and funded by Amgen, the company that makes tarlatamab—were presented October 20 at the annual meeting of the European Society for Medical Oncology (ESMO) in Madrid and published the same day in The New England Journal of Medicine (NEJM).
The new findings “support the use of tarlatamab in these previously treated patients,” said the trial’s senior investigator, Luis Paz-Ares, M.D., Ph.D., of Hospital Universitario 12 de Octubre in Madrid, who presented the results at the ESMO meeting.
The findings are “encouraging,” agreed Pilar Garrido, M.D., Ph.D., of Hospital Universitario Ramón y Cajal in Madrid, who spoke about the trial at the ESMO meeting but was not involved in it. However, she noted that patients need to be hospitalized to manage potentially serious side effects when they first receive the drug, which poses logistical challenges to its use.
Dr. Garrido also noted the need for more data on the effectiveness of tarlatamab against SCLC that has spread to the brain and for a biomarker that can predict which patients will respond to the drug.
According to Dr. Paz-Ares, the manufacturer of tarlatamab has already launched a large clinical trial comparing tarlatamab with standard chemotherapy in people with SCLC that has come back after one initial treatment.
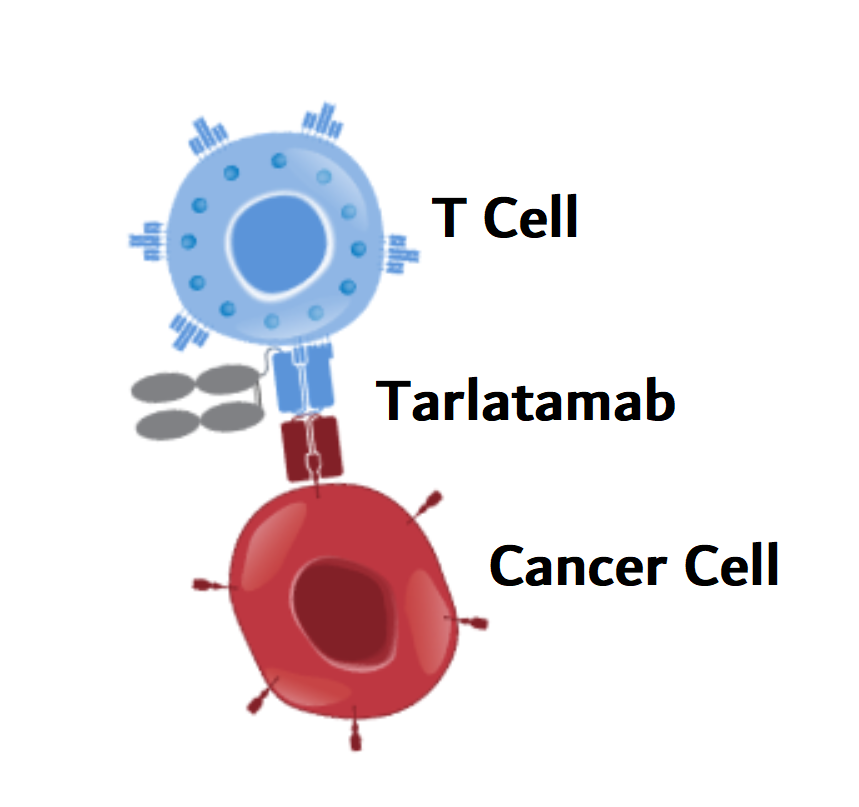
Tarlatamab harnesses T cells to destroy small cell lung cancer cells
Tarlatamab is a type of immunotherapy known as a bispecific T-cell engager, or BiTE. These two-armed drugs simultaneously latch onto tumor cells and immune cells called T cells. By bringing T cells and cancer cells close together, they help the T cell recognize and destroy the cancer cell.
The arm of tarlatamab that targets small cell lung cancer cells attaches to a protein called DLL3. This protein is normally located inside cells but is often present at high levels on the surface of SCLC cells, where it can be recognized by tarlatamab.
That makes DLL3 “a very attractive target in SCLC,” Dr. Garrido said.
The trial enrolled more than 200 people with advanced, or extensive-stage, SCLC that had progressed or was no longer responding to treatment. All of the participants had previously been treated with chemotherapy, and many had also been treated with an immune checkpoint inhibitor, a different type of immunotherapy drug. All participants had received at least two prior therapies, and one-third had received three or more.
The study team analyzed the response to tarlatamab in 100 participants who received 10 mg of tarlatamab by infusion every 2 weeks and another 88 who received 100 mg every 2 weeks. An additional 34 patients on the 10-mg dose were included in the analysis of side effects.
The 40% response rate (tumor shrinkage) seen in the 10-mg group “far exceeded” the 15% response rate that has historically been seen in people treated with standard therapies for SCLC that has relapsed, Dr. Paz-Ares and his colleagues wrote in NEJM.
Furthermore, 30% of those patients who responded to the drug had responses lasting at least 9 months. That finding is “exciting,” Dr. Thomas said, because the cancer usually grows so rapidly.
The median time that people in the 10-mg group lived after starting on tarlatamab was 14.3 months, compared with 6–12 months with current treatments. Researchers are still following the trial participants to learn more about tarlatamab’s side effects and its impact on how long people live.
Based on the initial results of DeLLphi-301, the lower (10 mg) dose of tarlatamab will be used in future clinical trials, Dr. Paz-Ares said.
Common and potentially serious side effects of tarlatamab
The side effects of tarlatamab were generally “manageable,” Dr. Paz-Ares said, and only about 3% of patients in the study stopped treatment entirely because of side effects. In addition, 13% of people in the 10-mg group and 29% in the 100-mg group had to temporarily pause treatment, have their dose reduced, or both, due to side effects.
The most common side effect of tarlatamab was cytokine release syndrome, a potentially life-threatening reaction in which inflammation spreads throughout the body. Other common side effects included decreased appetite, fever, and anemia.
About one-third of the patients experienced severe side effects, including serious cases of cytokine release syndrome. Severe side effects were more frequent in those receiving the higher dose of tarlatamab.
Most cases of cytokine release syndrome were “manageable and typically treated with supportive care,” such as intravenous fluids and drugs to control fever and inflammation, Dr. Paz-Ares said. However, one person in the 10-mg group died from respiratory failure resulting from treatment.
Another potentially serious side effect of tarlatamab is ICANS (immune effector cell−associated neurotoxicity syndrome), which includes a host of neurological effects such as severe confusion, attention problems, tremor, and muscle weakness. ICANS was more common in patients in the 100-mg treatment group and led one patient in each dose group to stop treatment entirely.
Both ICANS and cytokine release syndrome are commonly seen with immunotherapies that activate T cells to kill cancer cells, including other BiTEs and CAR T-cell therapy.
Challenges, concerns, and questions remain
Dr. Thomas noted that the trial was not designed to compare tarlatamab with standard therapy for SCLC. “But there is strong historical data on how quickly the disease progresses with standard therapy.”
Another issue, he said, is that current practice calls for treating all patients with extensive-stage SCLC with chemotherapy plus an immune checkpoint inhibitor at the time of diagnosis. However, about one in four people in the trial had not been treated with an immune checkpoint inhibitor. So it would be good to know how well tarlatamab works specifically for people whose cancer has come back despite previous immunotherapy, he explained.
Possible side effects are also a concern. There were few severe cases of cytokine release syndrome in the trial and most occurred after the first or second dose of tarlatamab. Still, the potential risk of side effects with early doses “is an important consideration,” Dr. Thomas said, because patients had to be hospitalized for a couple of days as a precaution when receiving each of the first two or three infusions of tarlatamab.
In addition, people had to be in generally good physical condition to participate in the trial, and the impact of potentially serious side effects could be greater in those who are sicker, he continued.
For all these reasons, Dr. Thomas said, it will be important to know “how we can best manage side effects such that we don’t need to admit patients to the hospital, and how we can anticipate, prevent, and treat side effects.”
He also pointed out that some patients died within 6 weeks after their treatment began, before the study team could assess if the deaths were due to worsening of the cancer. And “we need to better understand whether these early deaths were due to side effects,” he said.
Finally, Dr. Garrido said, another challenge is identifying biomarkers that can predict which patients are most likely to respond to tarlatamab. The research team looked at DLL3 on tumor cells as a potential biomarker, but whether a person responded to the drug did not appear to be linked to having DLL3 in their tumors, the study team reported.
“Despite the many challenges,” Dr. Garrido said, the results “offer renewed hope to our patients.”