, by NCI Staff
A study led by NCI researchers reinforces a recent idea that targeting an enzyme called WRN may be a new way to treat certain cancers. No existing drugs are known to specifically target the enzyme, but the NCI team—as well as several drug companies—are searching for one.
Last year, scientists discovered that cancer cells with a genetic feature called microsatellite instability-high (MSI-high) need WRN to survive. Getting rid of WRN killed MSI-high cancer cells but not healthy cells—sparking excitement about a potential new treatment approach.
Around 1 in 3 endometrial cancers, and 1 in 7 colorectal, stomach, and ovarian cancers, are MSI-high. It’s a hallmark feature of tumors that develop in people who have Lynch syndrome, a hereditary disorder that increases the risk of cancer. Specific tests can determine whether a person’s cancer is MSI-high.
The new study addresses the big question of why MSI-high cancer cells depend so heavily on WRN, said Sergei Mirkin, Ph.D., of Tufts University, who wasn’t involved in the study.
WRN unwinds unusual DNA structures that occur more frequently in MSI-high cancer cells than in other cancer cells, the NCI researchers found. In MSI-high cancer cells that lacked WRN, the structures eventually cause the DNA to shatter and the to cells die.
The findings, published September 30 in Nature, may change how cancer researchers think about microsatellite instability, said the study’s senior researcher, André Nussenzweig, Ph.D., of NCI’s Center for Cancer Research. Researchers from several other institutions also collaborated on the study.
DNA Breaks in MSI-High Cancer
Broken DNA. That’s what Niek van Wietmarschen, Ph.D., the study’s lead researcher, was awed by over and over again when he looked through the microscope at MSI-high colorectal cancer cells that were engineered to lack WRN.
“In 40% of the cells, the chromosomes look like dust,” Dr. van Wietmarschen said. “It’s like a bomb went off.”
He and his colleagues also noticed something else: The breaks occurred in the same areas in the genome, even in different kinds of lab-grown colorectal cancer cells. Nearly all of the breaks were near a long series of the same two DNA letters, or bases. The letters, T and A, were repeated back-to-back, as if there was a stutter in the DNA.
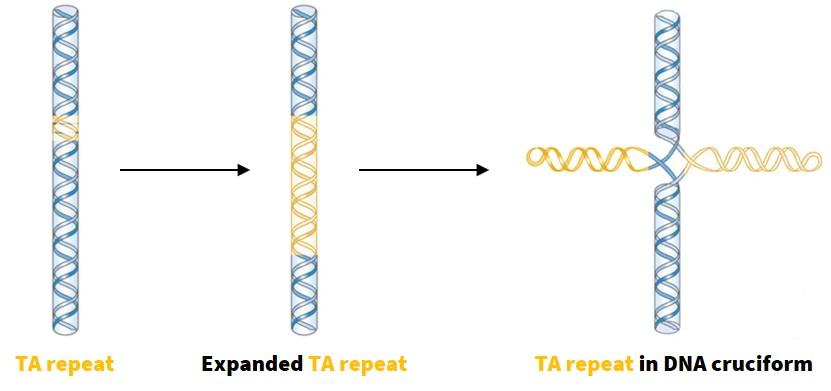
Repeats of back-to-back Ts and As are found in healthy cells and cancer cells without MSI, too. But in MSI-high cancer cells, many TA repeats were much longer than normal. Some were expanded several hundred times.
“I’d never seen anything like that before,” Dr. Nussenzweig said.
In fact, very few people have seen that before, Dr. Mirkin said. That’s because the standard way to read, or sequence, DNA skips over sections with long, repetitive sequences, he explained. But with new technologies, scientists can finally read these elusive sections of DNA.
“It’s becoming clear that [we] are missing too many important [DNA] elements” with the standard way of sequencing, Dr. Mirkin added. As researchers eventually shift to using the newer technologies, more features of DNA are likely to be discovered, he said. But at the moment, the new technologies are only available at a handful of large research institutions.
WRN Unravels Unusual DNA Structures
Next, the team explored why long TA repeats are more likely to break. Based on earlier studies of TA repeats, the researchers suspected it had something to do with the shape, or structure, of DNA in these sections.
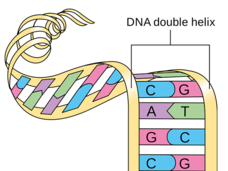
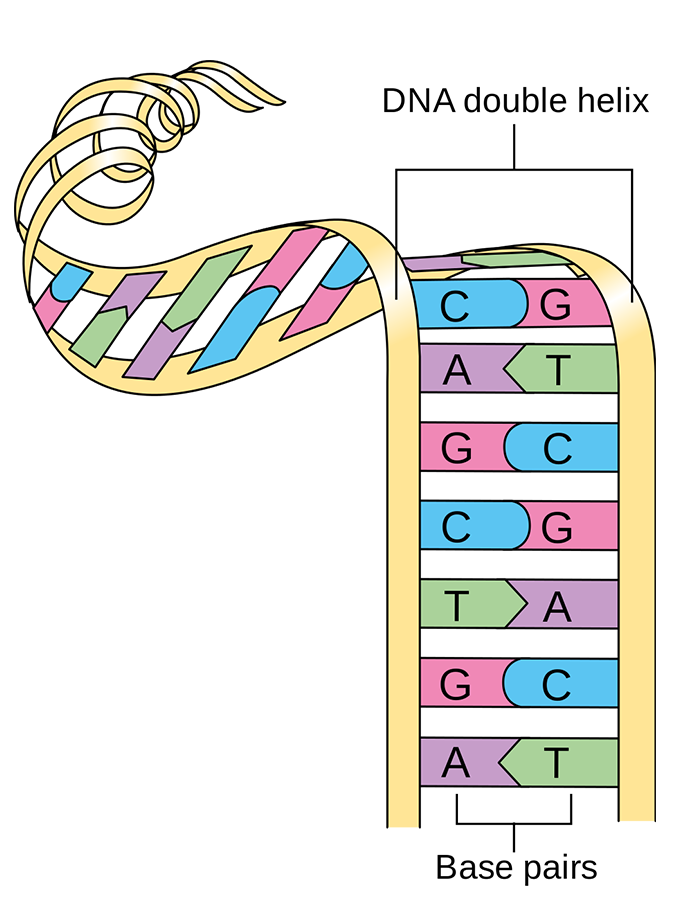
DNA is usually shaped like a ladder, with rungs connecting two sides. Normally, Ts and As on the opposite sides of the ladder link up, forming the rungs.
But if there are a bunch of Ts and As next to one another on the same side of the ladder, they can mistakenly connect with each other, forming an X-shaped structure called a DNA cruciform, Dr. Mirkin explained. More than 3 decades ago, he discovered that TA repeats readily form these structures.
In MSI-high cancer cells, long TA repeats did indeed form DNA cruciforms, the NCI researchers found. And that’s where WRN comes in. The enzyme’s job is to untangle these structures so that the DNA can get copied.
“If the structures aren’t teased out, DNA can’t get copied and the cell will eventually die,” Dr. Nussenzweig said.
WRN unwound DNA cruciforms in MSI-high cancer cells, the researchers showed. But in MSI-high cancer cells without WRN, other enzymes cut the DNA in a last-ditch effort to get rid of the structures.
Cells can typically recover from one or two DNA cuts. But in the MSI-high cancer cells lacking WRN, so many DNA cuts are made that chromosomes shatter and the cells die, Dr. Mirkin explained.
A New Treatment Idea for MSI-High Cancer
“Developing drugs that block WRN to treat MSI-high cancer is an exciting prospect,” Dr. Nussenzweig said.
That’s because while blocking WRN is unlikely to have much of an effect on healthy cells, “it’s super toxic in microsatellite unstable cells,” he said. That kind of relationship—where an existing defect makes the cancer cells especially susceptible to a specific treatment—is called synthetic lethality. It is especially sought out in cancer treatment approaches because it may cause fewer side effects by sparing healthy cells.
But Dr. Mirkin raised some concerns about blocking WRN. People with Werner syndrome, who are born without the WRN enzyme, age much faster and have a higher risk of cancer than people without the disorder, he pointed out. And DNA cruciforms can occur in healthy cells, so WRN is needed there, too. But cancer treatment is always a balance of benefits and harms, he said.
“Our findings may also provide a way to identify patients who might benefit from treatment with WRN-blocking drugs—even if the prospect of such a treatment is a long way down the road,” Dr. Nussenzweig said.
Because the elongated TA repeats occur in the same spots, even in different cancers, the researchers say they could be a sort of marker to tell if a person’s cancer is dependent on WRN—and may therefore benefit from treatment with a WRN-blocking drug.
The scientists are now working on developing a simple test for finding elongated TA repeats in patients’ tumors.