, by NCI Staff
Some patients diagnosed with advanced stomach (gastric) cancer may live longer if they are treated with the immunotherapy drug nivolumab (Opdivo) plus chemotherapy as an initial treatment, according to results from a large clinical trial.
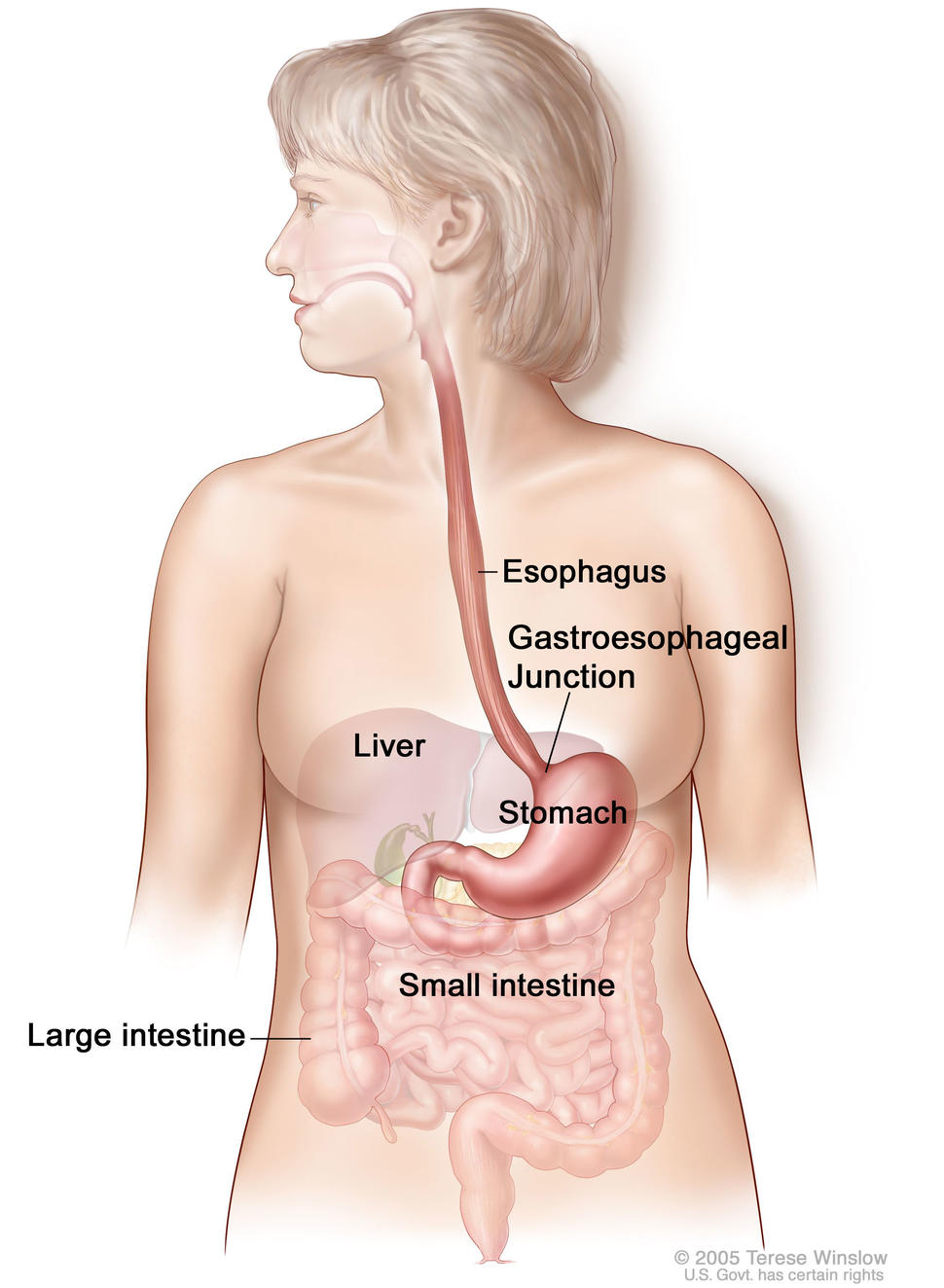
The international, multicenter trial, called CheckMate 649, included approximately 1,500 patients with advanced or metastatic stomach cancer that could not be removed by surgery. The study also included patients with gastroesophageal junction cancer, which occurs where the esophagus meets the stomach, and a cancer of the esophagus called esophageal adenocarcinoma.
The trial excluded patients whose tumors were known to be HER2-positive and who are typically treated with a therapy that targets HER2 along with chemotherapy.
Chemotherapy has been the standard initial treatment for patients with advanced or metastatic gastric or gastroesophageal junction cancer, according to Markus Moehler, M.D., Ph.D., of Johannes Gutenberg University Medical Center Mainz, who presented the trial results at the 2020 European Society for Medical Oncology (ESMO) virtual meeting on September 21.
Unfortunately, Dr. Moehler noted, most patients diagnosed with advanced stomach cancer have a poor prognosis and typically live for less than a year.
In the new study, the combination of nivolumab plus chemotherapy improved overall survival by several months and increased the length of time before the disease worsened (progression-free survival), compared with chemotherapy alone, Dr. Moehler said at the ESMO meeting.
The ESMO meeting also featured results from a second study evaluating nivolumab plus chemotherapy for advanced stomach cancer or gastroesophageal junction cancer. In the ATTRACTION-4 trial, the combination therapy improved progression-free survival versus chemotherapy alone. That study included 724 patients from Japan, South Korea, and Taiwan.
“Based on the results of these two trials, nivolumab plus chemotherapy will very likely become a standard first-line treatment for patients with these cancers,” said Carmen Allegra, M.D., who is special advisor to NCI’s Division of Cancer Treatment and Diagnosis on GI Cancer Therapies and was not involved in the trials.
A Possible Role for Immunotherapy Early in the Disease
Nivolumab binds to the protein PD-1 on T cells, which are a type of immune cell. By binding to PD-1, nivolumab prevents the protein from interacting with the PD-L1 protein on cancer cells and allows T cells to attack cancer cells.
Among patients with the highest PD-L1 levels in the CheckMate 649 trial, at a minimum follow-up of 12 months, the median overall survival was 14.4 months in the combination therapy group versus 11.1 months in the chemotherapy-alone group.
But the researchers also found more modest improvements in median overall survival among patients with lower PD-L1 levels and in the study population overall. Bristol Myers Squibb, the maker of nivolumab, sponsored the trial.
In the ATTRACTION-4 trial, with a median follow-up period of 11.6 months, median progression-free survival was 10.5 months in the combination-therapy group versus 8.3 months in the chemotherapy-alone group. The study was funded by ONO Pharmaceutical and Bristol-Myers Squibb.
Three years ago, Dr. Allegra noted, another checkpoint inhibitor, pembrolizumab (Keytruda), was approved for treating patients with advanced gastric cancer or gastroesophageal junction cancer that has worsened despite two or more types of treatment.
“We have known that there is a role for immunotherapy in treating gastric cancer in the later stages of disease,” said Dr. Allegra. “These new findings demonstrate that the approach can benefit patients as a first-line treatment.”
It’s not clear yet whether use of the combination therapy improves survival in patients whose tumors do not express PD-L1, he added, “although these data should [eventually] be available from both trials.”
The ATTRACTION-4 trial did not demonstrate that the combination treatment improved overall survival (a co-primary endpoint), but that may be because a substantial number of patients who initially received chemotherapy alone went on to receive an anti-PD-L1/PD-1 agent after the disease worsened during chemotherapy, Dr. Allegra pointed out.
“A Good Day for Patients with Gastric Cancer”
In both trials, the side effects of the combination therapy were similar to those reported previously in studies involving chemotherapy plus nivolumab in patients with other types of cancer.
“Most patients have few side effects and do very well with these immunotherapy drugs,” said Dr. Allegra. He noted, however, that some patients may develop inflammation in various organs that can lead to symptoms. Inflammation of the bowel, for example, can cause diarrhea. In rare cases, some types of immunotherapy may cause severe or even fatal allergic and inflammation-related reactions.
In the CheckMate 649 trial, 38% of patients discontinued the combination due to treatment-related side effects, compared with 25% of patients who received chemotherapy alone. In the combination-therapy group, 8 patients died as the result of treatment-related toxicity compared with 4 patients in the chemotherapy-alone group.
Elizabeth Smyth, M.D., of Addenbrooke’s Hospital in Cambridge, the United Kingdom, who discussed the two trials during the EMSO meeting, said, “It is a good day for patients with gastric cancer.”
The demonstration of a treatment regimen that could improve survival beyond one year was “a milestone,” Dr. Smyth added. More research, she went on, is needed to understand which patients may benefit most from the treatment based on biological markers such as PD-L1.
The CheckMate-649 is also evaluating the combination of nivolumab plus ipilimumab (Yervoy) compared with chemotherapy alone in patients with gastric cancer, gastroesophageal junction cancer, or esophageal adenocarcinoma.