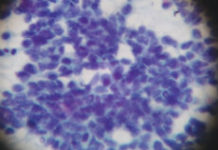
A melanoma cell. Credit: Dr Erik Sahai.
The National Institute for Health and Care Excellence (NICE) has recommended the use of the immunotherapy drug pembrolizumab (Keytruda) for some adults in England with a type of advanced melanoma skin cancer.
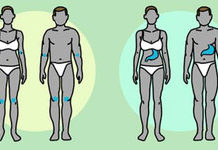
The drug will now be routinely available on the NHS to adults with stage 3 melanoma that’s spread to the lymph nodes and who have undergone surgery.
Until recently, patients’ only option was close monitoring after surgery, with other treatment options still very limited.
Current evidence shows that around 75% of people who take pembrolizumab after surgery do not have their cancer come back within a year of their treatment – a significant improvement on current standards.
Matt Sample, policy manager at Cancer Research UK, said: “This is good news for people who’ve had surgery for this type of skin cancer. Clinical trials have shown that pembrolizumab can reduce the risk of reoccurrence, meaning it has the potential of reducing the worries these people might have about their cancer returning.”
A need to prevent cancer from coming back
Melanoma is the 5th most common cancer in the UK, and around 7% of cases are diagnosed at stage 3. Around half the number of people diagnosed at this stage will survive their cancer for 5 years or more.
Cancer returning after treatment can significantly reduce chances of survival. As around 60 to 70% of these patients will have their cancer come back after surgery within 5 years, there has been a great need to develop new treatments that can prevent this.
“Fear of recurrence of cancer is also a huge emotional burden for patients and families and in particular for the growing population of melanoma patients who are diagnosed at a younger age, with the majority of their life ahead of them,” said Susanna Daniels, chief executive of Melanoma Focus.
Current evidence from a phase 3 clinical trial shows that around 75% of people who take pembrolizumab after surgery do not have their cancer come back within a year of their treatment.
As the trial is still ongoing to collect more data, the drug was previously only available through the Cancer Drugs Fund, which helps provide access to promising medicines while further evidence is gathered on its clinical and cost-effectiveness.
Whilst evidence now shows that pembrolizumab can prolong the amount of time someone can have before their cancer comes back, there is still not enough data to know whether the drug improves overall survival.
Despite this uncertainty, NICE believes that the benefit shown by the drug means it is still likely to be cost-effective, and so have approved it for routine use.
“I am delighted for patients that NICE have recognised the value this treatment adds for people with stage 3 melanoma by reducing the likelihood of recurrence, and that it will now be available on a routine basis,” added Daniels.
Pembrolizumab is an immunotherapy that aims to boost the immune system’s ability to recognise and kill cancer cells. It works by blocking a molecule found on immune cells – called PD-1 – from talking to cancer cells.
NICE decisions are usually adopted in Wales and Northern Ireland as well, so the decision is likely to affect patients in all 3 nations. Scotland has a separate process for reviewing drugs.