In a 20-year prospective follow-up study, Dr. Derk C.F. Klatte of the Leiden University Medical Center in Leiden, Netherlands and colleagues demonstrated that individuals with a germline CDKN2A pathogenic variant are at high risk of primary and second pancreatic ductal adenocarcinomas. This study encompasses the largest number of pancreatic ductal adenocarcinoma cases detected in pancreatic cancer surveillance to date, in which the outcomes are better than what is currently reported for individuals diagnosed with pancreatic ductal adenocarcinoma in the general population. The study outcomes support the evidence that pancreatic cancer surveillance in individuals at high risk leads to detection of early-stage, resectable pancreatic ductal adenocarcinomas with improved survival. The findings are published online on 3 June 2022 in the Journal of Clinical Oncology.
For high-risk individuals with a strong family history or carriers of specific germline pathogenic variants, evidence has accumulated that surveillance leads to detection of pancreatic ductal adenocarcinoma at an earlier stage, higher resectability, and improved survival. Although a recent cohort study found a substantial diagnostic yield of pancreatic ductal adenocarcinoma in carriers of high-risk pathogenic variants, surveillance did not evidently translate into improved outcomes, so effectiveness of pancreatic cancer surveillance is still under debate, the authors wrote in the background.
A surveillance programme for CDKN2A pathogenic variant carriers was initiated in 2000 at the Leiden University Medical Center. The majority of this population carries a specific Dutch founder pathogenic variant in CDKN2A known as p16-Leiden. CDKN2A/p16-Leiden pathogenic variant carriers are at 70% lifetime risk of melanoma and a 15-20% lifetime risk of pancreatic cancer. Evaluations of surveillance in this high-risk cohort have been previously published with key findings indicating increased resectability (75%) and survival (5-year survival rate of 24%) compared with pancreatic ductal adenocarcinoma in the general population. These results were promising, but it is important to evaluate if surveillance increases diagnosis of stage I pancreatic ductal adenocarcinoma, which is currently considered as a goal of beneficial pancreatic cancer surveillance programme.
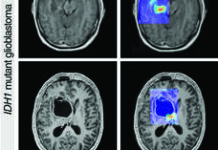
In the latest report, the study investigators present an update of their pancreatic cancer surveillance programme, in which they report on the yield and outcomes of a 20-year prospective follow-up of a unique and large cohort of germline CDKN2A pathogenic variant carriers. In addition, they assessed whether surveillance in this population leads to detection of early-stage pancreatic ductal adenocarcinoma with higher resection rates and improved prognosis. Surveillance consisted of annual magnetic resonance imaging with magnetic resonance cholangiopancreatography and optional endoscopic ultrasound.
In total, 347 germline pathogenic variant carriers participated in surveillance and were followed for a median of 5.6 years (interquartile range 2.3-9.9). A total of 36 cases of pancreatic ductal adenocarcinoma were diagnosed in 31 patients (8.9%) at a median age of 60.4 years (interquartile range 51.3-64.1). The cumulative incidence of primary pancreatic ductal adenocarcinoma was 20.7% by age 70 years. In 5 of 31 carriers (16.1%), a second primary pancreatic ductal adenocarcinoma was diagnosed.
In total, 30 of 36 pancreatic ductal adenocarcinomas (83.3%) were considered resectable at the time of imaging; 12 of 36 cases (33.3%) presented with stage I disease. The median survival after diagnosis of primary pancreatic ductal adenocarcinoma was 26.8 months, and the 5-year survival rate was 32.4% (95% confidence interval [CI] 19.1 to 54.8). Individuals with primary pancreatic ductal adenocarcinoma who underwent resection (22 of 31; 71.0%) had an overall 5-year survival rate of 44.1% (95% CI 27.2 to 71.3). The authors also reported that 9 of 347 individuals (2.6%) underwent surgery for a suspected malignant lesion, which proved to not be pancreatic ductal adenocarcinoma, and this included 5 lesions with low-grade dysplasia.
The authors commented that a major strength of their study is the prospective, long-term follow-up of a highly selected population of proven CDKN2A pathogenic variant carriers. These results add to the scarce data on outcomes of pancreatic cancer surveillance. Furthermore, surveillance was performed in a highly dedicated and experienced multidisciplinary team. Although this study records one of the longest follow-up so far, the majority of cases were diagnosed in the past decade. A benefit of surveillance seems to be particularly attainable in individuals with a proven pathogenic variant, who are at highest risk of developing pancreatic ductal adenocarcinoma.
Reference
Klatte DCF, Boekestijn B, Wasser MNJM, et al. Pancreatic Cancer Surveillance in Carriers of a Germline CDKN2A Pathogenic Variant: Yield and Outcomes of a 20-Year Prospective Follow-Up. JCO; Published online 3 June 2022. DOI: 10.1200/JCO.22.00194