In SPOTLIGHT, a global, randomised, placebo-controlled, double-blind, phase III study, zolbetuximab, a monoclonal antibody targeting claudin-18 isoform 2 (CLDN18.2) significantly prolonged progression-free survival (PFS) and overall survival (OS) when combined with mFOLFOX6 versus placebo plus mFOLFOX6 in patients with CLDN18.2-positive, HER2-negative, locally advanced unresectable or metastatic gastric or gastro-oesophageal junction adenocarcinoma. Prof. Jaffer A Ajani of The University of Texas, MD Anderson Cancer in Houston, TX, US and colleagues who published the findings on 14 April 2023 in The Lancet wrote that zolbetuximab plus mFOLFOX6 might represent a new first-line treatment in these patients.
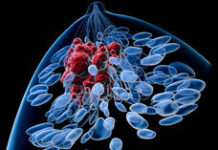
The authors wrote in the background that CLDN18.2 is a tight junction protein that is normally expressed exclusively in gastric mucosa cells. Its expression is retained in most gastric and gastro-oesophageal junction adenocarcinoma cells and is the dominant CLDN18 isoform expressed in both normal and malignant gastric cells. During malignant transformation, cell polarity is lost and CLDN18.2 might become exposed on the surface of gastric and gastro-oesophageal junction adenocarcinoma cells, which might render CLDN18.2 more accessible to antibodies, making it as a promising therapeutic target.
Zolbetuximab is a first-in-class chimeric immunoglobulin G1 monoclonal antibody that targets and binds to CLDN18.2. This binding mediates cell death of CLDN18.2-positive gastric and gastro-oesophageal junction adenocarcinoma cells via antibody-dependent cellular cytotoxicity and complement-dependent cytotoxicity. The phase IIb FAST study suggested that zolbetuximab improves PFS and OS when combined with first-line chemotherapy versus chemotherapy alone in patients with advanced gastric or gastro-oesophageal junction adenocarcinoma, The survival benefit was enhanced in patients whose tumours had higher CLDN18.2 expression.
SPOTLIGHT enroled patients from 215 centres in 20 countries. Eligible patients were aged 18 years or older with CLDN18.2-positive (defined as ≥75% of tumour cells showing moderate-to-strong membranous CLDN18 staining), HER2-negative, previously untreated, locally advanced unresectable or metastatic gastric or gastro-oesophageal junction adenocarcinoma, with radiologically evaluable disease (measurable or non-measurable) according to RECIST v1.1, an ECOG performance status 0 or 1, and adequate organ function.
Patients were randomly assigned (1:1) via interactive response technology and stratified according to region, number of organs with metastases, and previous gastrectomy. Patients received zolbetuximab (800 mg/m2 loading dose followed by 600 mg/m2 every 3 weeks) plus mFOLFOX6 (every 2 weeks) or placebo plus mFOLFOX6. The primary endpoint was PFS assessed by independent review committee in all randomly assigned patients. Safety was assessed in all treated patients. The study is closed to new participants.
Between 21 June 2018 and 1 April 2022, in total 565 patients were randomly assigned to receive either zolbetuximab plus mFOLFOX6 (283 patients; the zolbetuximab group) or placebo plus mFOLFOX6 (282 patients; the placebo group). At least one dose of treatment was administered to 279 of 283 patients (99%) in the zolbetuximab group and 278 of 282 patients (99%) in the placebo group. In the zolbetuximab group, 176 patients (62%) were male and 107 (38%) were female. In the placebo group, 175 patients (62%) were male and 107 (38%) were female. The median follow-up duration for PFS was 12.94 months in the zolbetuximab group versus 12.65 months in the placebo group.
Zolbetuximab treatment showed a significant reduction in the risk of disease progression or death compared with placebo (hazard ratio [HR] 0.75, 95% confidence interval [CI] 0.60–0.94; p = 0.0066). The median PFS was 10.61 months (95% CI 8.90–12.48) in the zolbetuximab group versus 8.67 months (8.21–10.28) in the placebo group. Zolbetuximab treatment also showed a significant reduction in the risk of death versus placebo (HR 0.75, 95% CI 0.60–0.94; p = 0.0053).
Treatment-emergent grade 3 or worse adverse events occurred in 242 of 279 patients (87%) in the zolbetuximab group versus 216 of 278 (78%) patients in the placebo group. The most common grade 3 or worse adverse events were nausea, vomiting, and decreased appetite. Treatment-related deaths occurred in 5 patients (2%) in the zolbetuximab group versus 4 patients (1%) in the placebo group. No new safety signals were identified.
The authors wrote that the results of SPOTLIGHT support that CLDN18.2 defines a large population of patients whose survival might be significantly prolonged by targeted therapy with zolbetuximab plus mFOLFOX6. Platinum–fluoropyrimidine chemotherapy is a standard first-line therapy for the large population of patients with HER2-negative disease; many of these patients also have disease with a PD-L1 combined positive score (CPS) less than 5. Zolbetuximab is being tested in other studies in CLDN18.2-positive gastric and pancreatic adenocarcinomas. SPOTLIGHT is the first phase III study to show a survival improvement after CLDN18.2-targeted therapy in any tumour type. Longitudinal assessments showed that the OS benefit in patients receiving zolbetuximab versus placebo was maintained over time. Survival continues to be followed-up in patients who remain on study.
In an accompanied editorial article, Drs. Hanneke W M van Laarhoven and Sarah Derks of the Department of Medical Oncology, Amsterdam UMC, University of Amsterdam, and Cancer Centre Amsterdam, Cancer Treatment and Quality of Life, both based in Amsterdam, Netherlands wrote that advances in biomarker-based targeted treatments have been slow for patients with stage IV gastro-oesophageal adenocarcinoma, with median OS for patients with HER2-negative disease not exceeding a year. Studies on the efficacy of combining chemotherapy with PD1 inhibitors have changed the standard of care for these patients.
The survival results reported by SPOTLIGHT investigators are unprecedented. However, not only patients who received zolbetuximab, did well. Patients who received chemotherapy only, had a median OS of 15.54 months, which is remarkably long for this disease. This finding could suggest that CLDN18.2 has prognostic power, but this has not been observed in previous studies.
Additional molecular analyses to characterise CLDN18.2-expressing tumours showed that 13% of assessed patients with CLDN18.2-positive cancers had a PD-L1 CPS of 5 or more, meaning that these patients could potentially benefit from both zolbetuximab treatment and PD1 inhibition. As the placebo group of the SPOTLIGHT study did not include PD1 inhibition in cases of PD-L1 CPS of 5 or more, it is unclear whether this population might benefit most from zolbetuximab, immune checkpoint inhibition, or a combination of both. These treatment regimens are being tested in the phase II ILUSTRO study.
In the SPOTLIGHT, the PFS and OS curves only started to separate after 6-9 months. This finding implies that around 20% of patients died before they could have benefited from the drug, whereas the major side-effects of zolbetuximab (nausea and vomiting) occurred in the beginning of the treatment period. Intriguingly, in the recent GLOW study, when comparing capecitabine and oxaliplatin (CapOx) to CapOx with zolbetuximab, early separation of the survival curves was observed, which could suggest that CapOx is a more favourable treatment regimen for combination with zolbetuximab. From a patient perspective, a treatment regimen once every 3 weeks might be preferably compared to chemotherapy once every 2 weeks and an antibody regimen once every 3 weeks.
Data are expected about alternative CLDN18.2-targeting strategies such as bi-specific antibodies, antibody drug conjugates, chimeric antigen receptor T-cell therapies, and novel antibodies with increased CLDN18.2 affinities, which might allow for lower dosing while retaining efficacy. Although some important questions remain unanswered about the best place for zolbetuximab in the treatment of gastric cancer, the SPOTLIGHT results indicate CLDN18.2 as a clear treatment target in gastric cancer according to the editorialists.
The study was funded by Astellas Pharma, Inc.
References
- Shitara K, Lordick F, Bang Y-J, et al. Zolbetuximab plus mFOLFOX6 in patients with CLDN18.2-positive, HER2-negative, untreated, locally advanced unresectable or metastatic gastric or gastro-oesophageal junction adenocarcinoma (SPOTLIGHT): a multicentre, randomised, double-blind, phase 3 trial. The Lancet; Published online 14 April 2023. DOI: https://doi.org/10.1016/S0140-6736(23)00620-7
- van Laarhoven HWM, Derks S. Claudin-18.2 targeting by zolbetuximab: results of SPOTLIGHT in perspective. The Lancet; Published online 14 April 2023. DOI: https://doi.org/10.1016/S0140-6736(23)00732-8