, by NCI Staff
For many people with chronic myelogenous leukemia (CML), the drug imatinib (Gleevec) changed a once-fatal blood cancer into a manageable disease and allowed them to live a nearly normal lifespan.
Until recently, imatinib and related drugs for CML, known as tyrosine kinase inhibitors (TKIs), had to be taken every day for life, and the drugs can cause fatigue, depression, disrupted sleep, diarrhea, and other side effects.
In 2018, based on results of two international studies, the Food and Drug Administration (FDA) approved an update to the recommended use of the TKI nilotinib (Tasigna) for CML. The update states that some people with CML who have been in remission for at least 3 years on nilotinib can safely stop taking the drug, although they must be closely monitored to make sure the cancer has not come back, or recurred.
New results from a US clinical study confirm these findings for nilotinib as well as for imatinib and two other TKIs. The study is also the first to show that patients’ quality of life improves after they stop TKI treatment. About two-thirds of patients in the study remained in remission from CML 3 years after stopping treatment and most of them were still in remission at the 4-year mark. Many reported improvements in common treatment-related symptoms, particularly fatigue and diarrhea.
“We had assumed that people with CML would feel better if they stopped treatment. Now we have hard data to back that up,” said Kendra Sweet, M.D., of the Moffitt Cancer Center and Research Institute, who was not an investigator on the new study but enrolled some patients on it.
“For CML patients who are in a sustained deep remission—with very low levels of leukemia cells in the blood for at least 2 years—it’s safe to stop treatment, and doctors should encourage their patients” to try stopping, said Ehab Atallah, M.D., of the Medical College of Wisconsin, who led the study.
The results, published November 12 in JAMA Oncology, could help motivate people newly diagnosed with CML to take their medication daily as prescribed, with the hope that they might safely stop taking the drugs entirely down the line, Dr. Sweet said.
Life After Stopping TKIs
The Life After Stopping TKIs (LAST) study enrolled 172 adults with CML from 14 university medical centers and cancer centers across the United States. Participants had CML that was well controlled with one of four TKIs used to treat the disease: imatinib, dasatinib (Sprycel), nilotinib, or bosutinib (Bosulif).
To be included in the study, patients had to have been taking a TKI for at least 3 years and to have stayed in a deep molecular response for at least 2 years, meaning that their test results showed almost no cells in the blood containing the genetic alteration that causes CML.
All participants stopped TKI treatment and were followed for at least 3 years by the researchers. Patients were monitored for recurrence with blood tests once a month for the first 6 months, every 2 months for the next 18 months, and then every 3 months after that.
At regular intervals during the study, participants were asked to report their symptoms, including fatigue, depression, diarrhea, sleep problems, and pain.
Three years after stopping TKI treatment, about 66% of participants (112 people) were still in remission. Those who stayed off treatment reported modest but meaningful improvements in fatigue, depression, sleep disturbance, and diarrhea—all symptoms that affect a person’s quality of life—that started within a year after stopping treatment.
And for many patients, “the quality of their day-to-day life is the most important thing,” Dr. Sweet said.
Patients whose blood tests showed that their disease had come back were restarted on TKIs and monitored for the rest of the study period. All patients who restarted treatment went back into remission, Dr. Atallah said.
Nine patients restarted treatment despite still being in remission, which Dr. Sweet said was the one “discouraging” aspect of the study. Most patients went back on a TKI either because of anxiety about being off treatment or because they developed a type of joint pain that is part of a TKI withdrawal syndrome.
“We don’t know why, but this joint pain happens in about 30% of patients [who stop TKIs and stay off them] and goes away in about 6 months,” Dr. Atallah said.
Predicting Who Can Successfully Stop Treatment
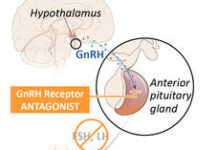
For the study, two different FDA-cleared lab tests were used to assess the levels of leukemia cells in patient blood samples—one a commonly used older test and the other a newer, more sensitive, more expensive test that is not yet widely available. Both tests rely on a technology known as polymerase chain reaction (PCR) to detect the genetic alteration that causes CML, a fusion of two different genes known as BCR-ABL.
Patients who had undetectable levels of BCR-ABL proteins by both tests at the time they stopped treatment were most likely to stay in remission, with only a 10% chance of their disease coming back during the 3 years they were off treatment, the researchers found. By contrast, patients with very low but detectable BCR-ABL proteins by one test but not the other when stopping treatment had a 50%–64% chance of disease recurrence over that time.
These “intriguing findings … suggest that patients with deeper [molecular] responses are more likely to be able to successfully discontinue therapy,” Theodore Braun, M.D., Ph.D., and Brian Druker, M.D., of the Knight Cancer Institute, Oregon Health & Science University, wrote in a commentary on the new study.
But because the more sensitive test, known as digital PCR, “is only available in a few centers and this was a relatively small study, additional … studies will be necessary” to validate these findings and ensure that they are more broadly applicable, Drs. Braun and Druker continued.
Curing CML Is the Ultimate Goal
Results of the LAST study and longer-term follow-up results from other recent studies of stopping TKIs in people with CML show that “most patients who are in remission will stay in remission, especially after they cross the 3-year mark” of being off treatment, Dr. Atallah said.
But only about 20%–25% of all CML patients can successfully stop taking the drugs and remain in remission for 3 years or longer, he said, and these patients still must be closely monitored.
“Ultimately, our goal is to cure patients with CML,” which ideally would mean being off treatment and having no evidence of disease for the rest of their lives, Dr. Atallah said.
Most people with CML don’t consider being on treatment forever the same as being cured, as a recent study led by LAST study co-investigator Kathryn Flynn, Ph.D., of the Medical College of Wisconsin found.
In addition to experiencing side effects that affect the quality of their day-to-day life, Dr. Atallah said, people who remain on a TKI for many years may have lasting damage to their kidneys, lungs, and liver.
Financial toxicity is also a concern, because the drugs are often costly even for patients who have health insurance.
For all these reasons, Drs. Atallah, Sweet, and colleagues at 19 research centers in the United States formed the H. Jean Khoury Cure CML Consortium. The consortium will test promising new treatment options for CML, such as drug combinations that could potentially eliminate leukemia stem cells from a patient’s bone marrow for good.
Key questions that remain about stopping TKIs, Dr. Atallah said, include figuring out why some patients can successfully stop treatment and others cannot, as well as how to better predict early on who can stop the drugs successfully. Understanding the reasons why some people can safely stop the drugs could also lead to new, improved treatments, he said.