“Over the last 30 years or so, I have noticed an increase in the number of young, fit people, who don’t have the associated risk factors, being diagnosed with bowel cancer,” says Dr Leslie Samuel, consultant oncologist in NHS Grampian.
“It got me thinking about whether antibiotic use could be a contributing factor towards these cases, as so many of us are exposed to antibiotics these days.”
Nearly 120 people will be diagnosed with bowel cancer, cancer that starts in the large bowel (the colon) and the rectum, every day in the UK. Of these cases, 54% are identified as ‘preventable’ cancers.
Factors associated with an increased risk of bowel cancer include eating processed meats, being overweight or obese, smoking, and drinking alcohol.
Bowel cancer is also more common in older people. However, over the last few decades, specialists like Samuel began to notice this unusual trend.
Since the 1990s, the rate of bowel cancer has more than doubled among adults younger than 50 in America. While in the UK, bowel cancer incidence rates increased by 50% in people aged under 50. This went from a 4.5 per 100,000 people average between 1993 and 1995, to a 6.7 per 100,000 people average between 2016 and 2018.
Samuel, working alongside Sarah Perrott from the University of Aberdeen, decided to investigate the rising tide in early onset bowel cancer and the potential role antibiotics could play.
They recently published the results of their study in the British Journal of Cancer, which found that antibiotic use may increase the risk of developing bowel cancer in the colon.
Another piece of the puzzle
The team, funded by us, analysed data from 7,903 people with bowel cancer and compared them to more than 30,000 matched people without a cancer diagnosis.
Although the research suggested that there was no link between antibiotics and rectal cancer, the study found that antibiotic usage was associated with 445 cases of bowel cancer in those less than 50 years of age. While it’s important to remember that these figures are still relatively low, these results may have pointed us to another piece of the puzzle.
“We found antibiotic exposure was associated with colon cancer among all age groups, but not with rectal cancer” says Perrott. “This, along with multiple other dietary and lifestyle factors, may be contributing to increased cases of bowel cancer among young people.”
What’s more, the team went on to analyse the data from a small subgroup of those that had developed early onset bowel cancer and found that cancer that developed in the right-hand side of the bowel was more highly associated with antibiotic use than the left hand side.
“The right hand side of the bowel has greater diversity of bacteria,” says Perrott. “So it all makes sense when we think about the contents of the bowel, the activity of the gut microbiome and the theory of bowel cancer development”.
‘Think of a meadow’
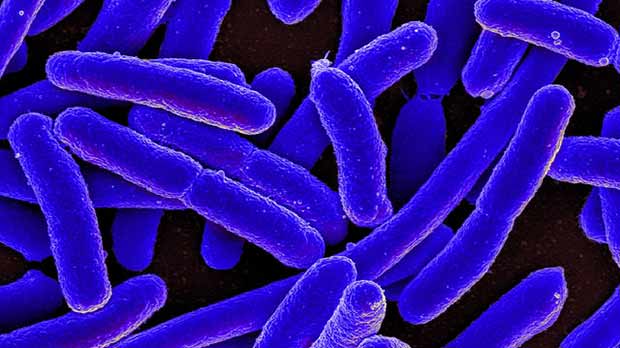
People say there are more stars in the universe than grains of sand on earth, more sheep than people in New Zealand and more bacteria in our bodies than human cells.
A lot of those bacteria are living in our gut.
This vibrant community, known as the microbiome, can help protect us from harm as well as providing nutrients for our cells. But certain bacteria have been linked to a host of different diseases from diabetes and mental health to cancer.
The link between the gut microbiome and bowel cancer (also known as colorectal cancer) has been researched for a while now and the theory behind these latest results is that the gut microbiome is impacted when you take antibiotics, a process known as dysbiosis.
“If you think of a meadow with lots of different wild grasses and flowers, if we were to then spread down weed killer, it would kill specific species, but not all of them,” explains Perrott.
“This would then upset the natural biodiversity of the meadow. As a result, for example, more weeds might grow because there’s less competition. We don’t like weeds – they might block out the sun for other wildflowers, they might change the pH of the soil, and continue to disrupt the meadow.”
Perrott explains that a similar situation occurs with antibiotics – they can selectively kill off certain types of bacteria living in the bowel. This can lead to other strains of bacteria become dominant, and upsetting the natural balance in our gut, which helps keep our bowel healthy and contribute to normal immune function. In theory, it’s this imbalance which might lead to chronic inflammation and an increase the risk of cancer.
Although this is a potential mechanism, we have barely begun untangling the complex eco-system that exists inside our bowel. We still have a lot to understand about which antibiotics might increase the risk.
“Antibiotic exposure is very common, and of course not everyone who’s exposed to antibiotics get bowel cancer,” Perrott adds. “We want to emphasise that antibiotics are very, very important drugs, but they should be used carefully and when use is necessary.”
What else do we know so far?
Samuel and Perrott aren’t the first people to explore this relationship.
A few years ago, Dr Cindy Sears, based on the east coast of America published a paper in the journal Gut, which saw a similar trend to that reported by Samuel and Perrott.
“I think it is impressive that the primary research studies have been largely consistent, not necessarily in the fine details, but in the overall concept that antibiotic exposure, at a distance from the diagnosis of bowel cancer, is associated with the disease,” says Sears.
Sears’ paper in 2019 used data over more than two decades, allowing us to see over a much longer timeframe how antibiotics might affect cancer risk.
Interestingly, the association with antibiotics “was only seen when the antibiotics were taken 10 years earlier than the onset of the cancer,” says Sears. “And the reason that’s an appealing number, which just came out of the data, is because that’s the magic number that people talk about, in terms of the time from a cell going bad in the epithelium in the colon and ability of the GI doctors to see bowel tumors on colonoscopy”.
Now, this particular paper from Samuel and Perrott has aligned with what many of us have wondered given the explosion of antibiotic use in the 1980 to 1990’s.”
The work from Samuel and Perrott is adding to a plethora of existing research.
The nuances with these results become important as it adds to the drumbeat of why use of antibiotics should be done well. Antibiotics are lifesaving. But the issue we’ve had is we became very lax.
Dr Cindy Sears
The issues with overuse of antibiotics are widespread – antibiotic resistance being one of the most discussed and pressing problems. And while these data strengthen the argument that antibiotic use needs to be reserved for situations where there’s an actual need, both Perrott and Sears are quick to emphasise just how important antibiotics are.
“Ultimately, this research really is part of a broader conversation about the gut microbiome and gut health,” says Samuel.
The bigger picture
There’s still so much to learn about the microbiome, but we are making real inroads.
Through Cancer Grand Challenges, we’re supporting an international group of scientists investigating how the microbiome drives bowel cancer, and whether we can manipulate it to find new routes to prevention and treatment.
While this programme is not investigating the link between antibiotics and bowel cancer, it is probing other important aspects of the microbiome, including looking for patterns that are associated with cancer development that may be linked to an increase in early onset bowel cancer. Sears is part of the team taking on the challenge of the microbiome, bringing her expertise in infectious disease.
With the wider global research community taking a greater interest in the microbiome, “we now have a range of studies looking into its association with bowel cancer, and people are asking the questions in different populations,” says Sears.
“The next key step is working out how we can convert everything we’ve learnt into prevention.”
Lilly