, by NCI Staff
Immunotherapy may become part of early treatment for some people with advanced esophageal cancer, based on results from two large clinical trials.
In both trials, treatment with drugs known as immune checkpoint inhibitors increased how long people with advanced esophageal cancer lived without their cancer getting worse, compared with those who received standard treatments. In one of the studies, people who received a checkpoint inhibitor also lived longer overall.
Findings from both trials were presented last month at the European Society for Medical Oncology (ESMO) virtual annual meeting.
The results from both studies are considered preliminary because the trials are still ongoing. But according to several experts on esophageal cancer, the results from both trials may lead to these drugs becoming new standard treatments for a cancer for which new, effective therapies have been hard to come by.
Using Pembrolizumab Early in Treatment
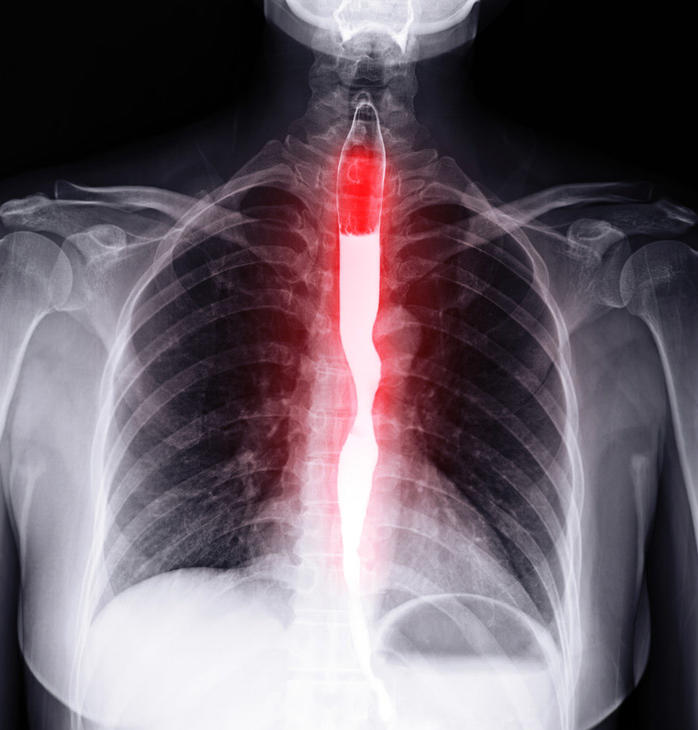
Esophageal cancer is often diagnosed at an advanced stage, when it has spread to nearby organs. If the disease has spread widely, a surgeon may not be able to remove all of the cancer and surgery won’t help the patient live longer. So standard initial (first-line) treatment consists of systemic treatment with chemotherapy.
Chemotherapy can cause some advanced esophageal tumors to shrink or stop growing for a while. However, the cancer usually gets worse or spreads within a few months.
“Esophageal cancers have a very poor prognosis, and 5-year survival in Western countries ranges between 10% and 12%,” said Andrés Cervantes, M.D., Ph.D., an oncologist at the University of Valencia in Spain who was not involved with either study, speaking at the ESMO meeting.
In 2019, the Food and Drug Administration (FDA) approved the immunotherapy drug pembrolizumab (Keytruda) as second-line treatment for some people with a type of locally advanced or metastatic esophageal cancer called esophageal squamous cell carcinoma (ESCC). This type of esophageal cancer most often arises in the lining of the upper or middle part of the esophagus.
“Esophageal cancer is an aggressive disease, more than some other common cancer types. Patients tend to be sicker when we first see them compared to patients with other tumor types,” explained Harry Yoon, M.D., of the Mayo Clinic, who was not involved in either trial. “So, when the cancer grows, approximately half of patients are typically not able to move on to a second-line therapy.”
Both of the clinical trials presented at the ESMO meeting were launched to test whether immunotherapy can improve how long patients live if given earlier in treatment.
The KEYNOTE-590 trial included about 750 people with esophageal cancer that had spread to nearby tissue or lymph nodes and couldn’t be removed with surgery. The study—which was funded by Merck, the manufacturer of pembrolizumab—included both people with ESCC and esophageal adenocarcinoma, which usually arises lower in the esophagus, closer to the stomach.
Participants were randomly assigned to receive treatment with either pembrolizumab plus the chemotherapy drugs 5-fluorouracil (5-FU) and cisplatin, or a placebo plus the chemotherapy drugs. In the trial, treatment with 5-FU and pembrolizumab or 5-FU and placebo could continue for up to 2 years, or until the cancer progressed.
Even though the trial is still ongoing, a difference had already emerged in how long people lived by the time of the ESMO presentation. Overall, people receiving chemotherapy plus pembrolizumab lived for a median of 12.4 months, compared with 9.8 months in those receiving chemotherapy plus placebo. The addition of pembrolizumab also modestly slowed the time to tumor progression.
People with high levels of a protein called PD-L1 on their tumors lived even longer after immunotherapy: a median of 13.5 months versus 9.4 months, respectively. PD-L1 is a protein that can be found on cancer cells and influences the response to pembrolizumab.
About 20% of people receiving immunotherapy plus chemotherapy stopped treatment because of side effects, compared with about 12% of people receiving chemotherapy plus placebo. In the immunotherapy group, 2.4% experienced side effects thought to have contributed to their death, compared with 1.4% who received chemotherapy alone, reported Ken Kato, M.D., Ph.D., of the National Cancer Center Hospital in Tokyo, Japan, who presented the KEYNOTE-590 trial results at ESMO.
“Pembrolizumab plus chemotherapy should be a new standard of care as first-line therapy in patients with locally advanced and metastatic esophageal cancer,” said Dr. Kato.
Dr. Yoon called the results “practice changing” for people with ESCC. Immunotherapy can also help patients with esophageal adenocarcinoma live longer, he added, “but clinicians may disagree on whether that applies to all [patients with adenocarcinoma].”
Patients with esophageal adenocarcinoma were underrepresented in KEYNOTE-590 compared with people with ESCC, added Dr. Cervantes. “So the impact [of first-line pembrolizumab] for adenocarcinomas may be contentious.”
Testing Nivolumab for Operable Esophageal Cancer
For some people with advanced esophageal cancer that has not spread widely, surgery may help them live longer. These people often undergo a grueling regimen of chemotherapy and radiation therapy to shrink the tumor before the operation (neoadjuvant treatment).
But, like people with inoperable esophageal cancer, “we’re dealing with a population of patients [whose cancer] may progress very quickly” after treatment, explained Ronan Kelly, M.D., from Baylor University Medical Center, who presented results from the second trial, called CheckMate 577, at ESMO.
Additional chemotherapy after surgery (adjuvant therapy) hasn’t been shown to help delay the cancer from returning, and most people are too weak after surgery to tolerate its side effects, he added.
Another immunotherapy drug called nivolumab (Opdivo) has been approved by FDA as a second-line treatment for advanced esophageal squamous cell cancer that can’t be removed surgically. Nivolumab targets the same immune checkpoint protein as pembrolizumab, PD-L1.
CheckMate 577 was launched to see if giving nivolumab immediately after surgery as adjuvant therapy can extend how long patients with locally advanced esophageal cancer live without their cancer coming back. The trial—which was funded by Bristol Myers Squibb, nivolumab’s manufacturer—included almost 800 people who had received chemotherapy, radiation therapy, and surgery for their cancer. Over half of participants had esophageal adenocarcinoma.
After neoadjuvant therapy and surgery, the participants were randomly assigned to receive nivolumab or a placebo for 16 weeks and could continue treatment for up to a year unless their cancer progressed.
CheckMate 577 is also still ongoing, but at the time of the ESMO presentation, people who received nivolumab immediately after surgery lived for a median of almost 2 years without their cancer progressing, compared with 11 months for those who received a placebo. Similar results were seen regardless of whether participants’ tumors had high or low levels of PD-L1, Dr. Kelly reported.
Participants are still being followed to evaluate the effects on overall survival.
More people who received nivolumab stopped treatment due to side effects compared with those who received a placebo: 9% versus 3%. No deaths due to treatment were recorded in either group.
Although preliminary, these results “represent the first treatment advance in many years for patients with operable esophageal or gastroesophageal junction cancer, potentially establishing adjuvant nivolumab as a new standard of care for these difficult-to-treat tumors,” Dr. Kelly added.
More work is needed to understand why differences in response to immunotherapy can be so stark: Some people don’t benefit at all from immunotherapy, while others can live for years, Dr. Yoon explained.
“Answering that question is an active area of research,” he said. “But immunotherapy has [now] pretty consistently shown that it has a key role in esophageal and gastric cancer.”