, by NCI Staff
People with thyroid or lung cancer whose tumors contain specific alterations in a gene called RET now have a new treatment option.
On May 8, the Food and Drug Administration (FDA) granted accelerated approval for the drug selpercatinib (Retevmo) to treat certain patients with RET-altered thyroid cancer or non-small cell lung cancer. The drug works by blocking the activity of RET proteins.
The drug’s approval was based on a study in which it shrank tumors in more than half of all patients with advanced RET-altered lung and thyroid cancers, in many cases for 6 months or longer. Selpercatinib, which is taken as a pill, appears to have fewer side effects than older drugs that block RET activity.
The study of selpercatinib, a clinical trial known as LIBRETTO-001, was sponsored by Eli Lilly and Company and Loxo Oncology, the original maker of the drug (now Loxo Oncology at Lilly).
Selpercatinib, the first drug to selectively target RET, is “an important development for the treatment of RET-altered cancers,” said Jaydira del Rivero, M.D., an oncologist specializing in endocrine cancers in NCI’s Center for Cancer Research, who was not involved in the study.
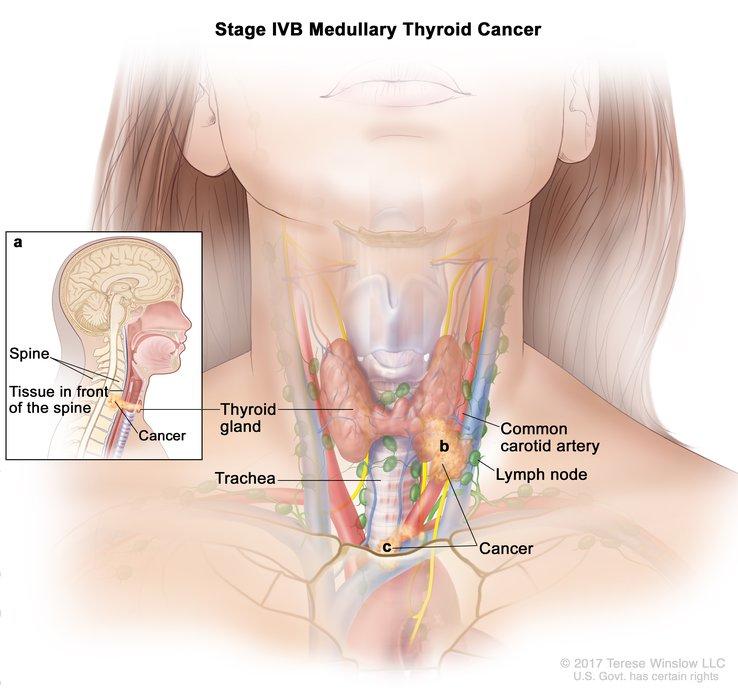
Under the approval, selpercatinib can be used in three groups of patients with RET-altered cancers: adults with non-small cell lung cancer that has spread, or metastasized; adults and children 12 years old and older with advanced or metastatic medullary thyroid cancer who require systemic therapy; and adults and children 12 years old and older with advanced or metastatic papillary thyroid cancer that is resistant to treatment with radioactive iodine and who require systemic therapy.
An accelerated FDA approval is designed to speed the availability of drugs that treat serious conditions and fill an unmet medical need. The approval of selpercatinib was based on the drug’s ability to shrink tumors and the duration of that response. Further studies are required by FDA to confirm that the treatment provides a clinical benefit to patients, such as by improving how long they live.
RET Alterations Spur Cancer Growth
RET alterations are rare in cancer overall but more common in lung and thyroid cancers. About 2% of people with non-small cell lung cancer and 10%–20% of those with papillary thyroid cancer, the most common type of thyroid cancer, have tumors in which a piece of the RET gene is fused to part of another gene, known as RET fusion–positive cancer. In addition, smaller genetic alterations (mutations) in RET are found in more than half of all cases of medullary thyroid cancer.
Although medullary thyroid cancer is rare, the outlook for people with this form of thyroid cancer is worse than for people with papillary thyroid cancer, said LIBRETTO-001 study investigator Lori Wirth, M.D., of Massachusetts General Hospital.
RET gene fusions and mutations result in the production of abnormal RET proteins, which spur the growth of cancer cells. RET is a type of protein called a kinase, which is involved in various cell processes.
Selpercatinib “was designed to target RET while minimizing its activity against other kinases. Most of the other drugs now in our arsenal that have some activity against RET-altered cancers are multi-kinase inhibitors that target and block the activity of other kinases” in addition to RET, Dr. Wirth said.
Although these other drugs, including cabozantinib (Cabometyx) and vandetanib (Caprelsa), have some activity against these cancers, their usefulness in treating RET-altered cancers is limited by their side effects. Because these earlier drugs block multiple kinases, the likelihood of side effects is higher than it is with the selpercatinib, she explained.
Clinical Study Results for Patients with Lung and Thyroid Cancer
The LIBRETTO-001 trial was launched to test selpercatinib in people with RET-altered cancers, and all participants in this phase 1/2 trial received the study drug.
Results for 105 patients with RET fusion–positive non-small cell lung cancer who had prior treatment with chemotherapy were described in an earlier Cancer Currents post. Among a second group of 39 patients with RET fusion–positive lung cancer who had not been treated previously, 85% responded to the drug—that is, their tumors shrank—and 58% of those patients had responses lasting 6 months or longer.
The trial also enrolled 55 patients with RET-altered medullary thyroid cancer who had previously been treated with cabozantinib, vandetanib, or both, as well as 88 who had not received these drugs. The response rates were 69% and 73% in the prior-treatment and no-prior-treatment groups, respectively, and in most patients the responses lasted 6 months or longer.
For the 19 patients in the study with RET fusion-positive thyroid cancer whose disease was no longer responding to radioactive iodine treatment and had received previous systemic treatment and 8 patients who had received only radioactive iodine, the response rates were 79% and 100%, respectively. These responses lasted 6 months or longer in many patients.
“Not only did we see high response rates, but the responses were also very long-lasting,” Dr. Wirth said. Investigators are continuing to follow patients in the study, and most patients who initially responded to the drug are still responding, she said.
The most common side effects of selpercatinib included diarrhea, high blood pressure, and increased blood levels of two liver enzymes—a sign of liver toxicity. Serious side effects, including abnormal heart rhythms and pneumonia, occurred in one-third of all patients in the study.
While most side effects could be managed, 5% of patients stopped treatment permanently because of serious side effects.
A Promising Option for Cancers with RET Alterations
“It’s not just that we have a new drug to help treat our patients with RET-altered thyroid cancers, but the drug has really good activity and a good side-effect profile” compared with other FDA-approved treatments for thyroid cancer, Dr. Wirth said.
Also important, Dr. del Rivero said, is that selpercatinib shrank thyroid tumors containing a the RET V804 mutation, which are resistant to other therapies.
It’s still not known if selpercatinib will help patients live longer, she continued. But she said the results so far suggest that the drug will eventually become the first-line treatment for people with RET-altered cancers, especially medullary thyroid cancer.
“More information is needed, but we are optimistic about this treatment,” Dr. del Rivero added.
To help provide this additional information, Eli Lilly has launched a phase 3 clinical trial that will compare selpercatinib with either cabozantinib or vandetanib in people with advanced, RET-mutated medullary thyroid cancer. However, Dr. Wirth said, the COVID-19 pandemic has temporarily slowed or halted enrollment of patients into the trial at some study sites, including her hospital.
Finally, Dr. Wirth said, “Now that we have a really good RET-specific therapy, we need to make sure that doctors and patients know” that it’s important to do genomic testing on tumor samples from patients with medullary thyroid cancer, to find out if they contain alterations in RET.