All cancer treatments have a common aim: to destroy tumour cells or keep them under control. Ideally, they cause tumours to shrink, but drugs can also be considered successful if they stop tumours growing.
However, the effects don’t always last forever. Sometimes a drug can have an initial impact on a cancer’s size or growth, but then the tumour starts to grow again.
It’s a phenomenon scientists are keen to tackle. And a group of our scientists may be making inroads on how cancer cells dodge the effects of a group of cancer drugs called PARP inhibitors.
These findings, published today in Nature Cell Biology, could lead to more effective treatments and eventually help in predicting who is likely to respond best to these widespread and important precision treatments.
It’s important to understand the mechanisms behind resistance so that we can make the drugs we already have work better and for more people.
– Michelle Mitchell, chief executive of Cancer Research UK.
What do we already know about PARP inhibitors
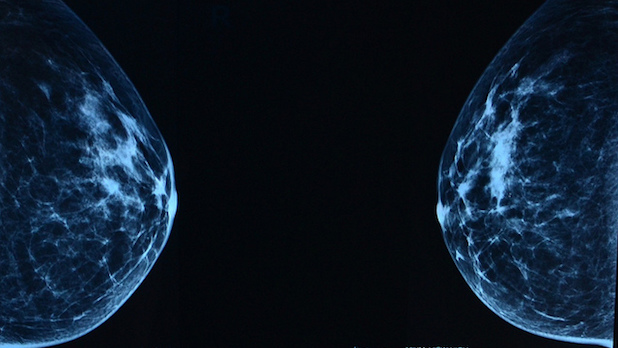
PARP inhibitors are a type of targeted cancer drug used to treat thousands of cancer patients, including those with breast, ovarian, pancreatic or prostate cancers, usually in people who have a fault known as a BRCA mutation.
This type of precision medicine is well known in the world of cancer treatment and includes common cancer drugs, such as olaparib and rucaparib. Olaparib alone has treated more than 30,000 patients.
“PARP inhibitors are one of the most exciting classes of precision medicine in cancer treatment today,” says Professor Chris Lord, who led the latest study. “But we are only now gaining a fuller understanding of why they work in some patients but not in others.”
PARP inhibitors block a key process inside cells – their ability to repair DNA. Latching on to a protein called PARP1, one of many DNA repair tools, the drugs render it inactive and trap it on the DNA. Not only does this stop DNA repair, but the trapped PARP1 then keeps building up until it poisons the cancer cell, eventually causing it to die.
These drugs have been found to be particularly effective in people whose cancer cells already have problems repairing DNA – including those with faults in the BRCA1 and BRCA2 genes.
But PARP inhibitors don’t work for everyone.
In fact, it’s estimated over 40% of patients with a faulty BRCA1 or BRCA2 gene don’t respond to the treatment. In some cases, this could be because cancer cells find a way to deal with the flood of trapped PARP1, making the treatment less effective.
At The Institute of Cancer Research in London, Lord and his team used innovative cell lines and protein analysis techniques to understand how resistance was unfolding.
A new understanding of PARP resistance
The team hunted for proteins that attached to PARP1 only when it was trapped to the DNA. They then analysed the most common candidates to better understand exactly how they make the cancer resistant.
Their hunt was fruitful. The team identified a small molecule known as p97, which was seen to play a crucial role in prying PARP off the DNA and rescuing the cancer cells from dying.
Using a mini tumour built with tissue from a triple negative breast cancer patient with a BRCA1 mutation, they discovered that blocking p97 made the cancer cells much more vulnerable to the PARP inhibitor talazoparib.
Results found that while a dose of talazoparib alone killed about 30% of the mini tumour, that figure increased to 90% when coupled with the p97 inhibitor. These significant results could unlock the key to tackling treatment resistance.
“Now that we have uncovered p97’s role in controlling PARP inhibitor resistance, we could, in future offer treatments that could save many more lives,” says Lord.
A new understanding of PARP resistance
The team hunted for proteins that attached to PARP1 only when it was trapped to the DNA. They then analysed the most common candidates to better understand exactly how they make the cancer resistant.
Their hunt was fruitful. The team identified a small molecule known as p97, which was seen to play a crucial role in prying PARP off the DNA and rescuing the cancer cells from dying.
Using a mini tumour built with tissue from a triple negative breast cancer patient with a BRCA1 mutation, they discovered that blocking p97 made the cancer cells much more vulnerable to the PARP inhibitor talazoparib.
Results found that while a dose of talazoparib alone killed about 30% of the mini tumour, that figure increased to 90% when coupled with the p97 inhibitor. These significant results could unlock the key to tackling treatment resistance.
“Now that we have uncovered p97’s role in controlling PARP inhibitor resistance, we could, in future offer treatments that could save many more lives,” says Lord.
What’s yet to come?
One of the compounds used to block p97 was disulfiram, a drug that’s used to help people cope with alcohol addiction.
For Lord and his team, the next challenge is to translate their new understanding of PARP inhibitor resistance into a way to predict which patients should be treated with PARP inhibitors, and who would be better off getting a different cancer treatment.
“Using new combinations of drugs that are already available is a smart way to get one step ahead of cancer, and we will need more research to know how effective this approach might be for PARP inhibitors. But the findings from this study are a promising new way to stack the odds in the patient’s favour, by offering treatment which works best for them,” says Mitchell.
Lilly








