 9 years, £14 million, 19 centres across the UK, 250 researchers and clinicians, and over 800 people with non-small cell lung cancer (NSCLC).
9 years, £14 million, 19 centres across the UK, 250 researchers and clinicians, and over 800 people with non-small cell lung cancer (NSCLC).
If you’d asked for a description of TRACERx, our flagship lung cancer study, those numbers would be just scratching the surface.
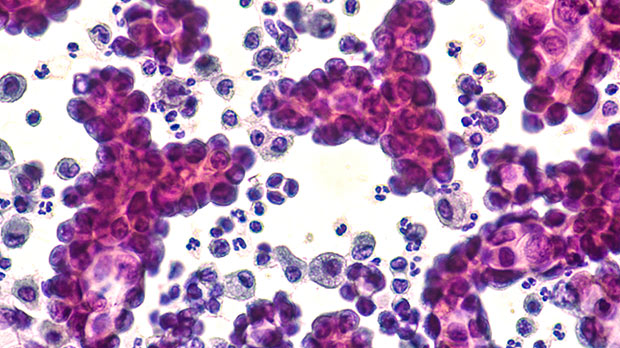
Lung cancer is the third most common cancer in the UK. Around 48,500 people are diagnosed in the UK each year. Of these, around 80 to 85% are NSCLC.
Since 2014, TRACERx has been collecting comprehensive genomic and clinical data from people with NSCLC, from their point of diagnosis throughout their treatment, to unpick the complexities of lung cancer and aid the design of new, targeted lung cancer treatments.
Today, researchers based at the Francis Crick Institute have published 7 papers in the journals Nature and Nature Medicine, detailing new results from TRACERx.
Each of these papers is revealing the secrets of how lung cancer can evolve, spread and resist treatment, from how the visual characteristics of lung tumour cells may indicate a person’s prognosis to how DNA from ancient viruses can be reactivated in tumours to accelerate their growth.
TRACERx recognises that cancer is not static and the way we treat patients shouldn’t be either.
– Professor Charles Swanton, TRACERx lead researcher
The evolutionary tree
The DNA in a tumour can greatly differ from cell to cell. This results in smaller clusters of different cells within a tumour, giving a tumour something called intratumour heterogeneity (ITH). ITH is one of the things that make it easier for cancers to evolve and develop treatment resistance.
As the tumour grows, it’s DNA continues to mutate, and a new cluster of genetically different cells, called a subclone, can form.
Think of it like a tree. The initial tumour cells form the trunk, and each time a cell mutates enough to begin to form a subclone, it branches off. That can happen multiple times, resulting in more and more branches of the tree, and can even happen within branches, creating further offshoots of new subclones.
However, not all subclones will continue to develop and form new ones. The ones that do are said to be ‘selected for’, meaning one or more of the mutations it has developed help it to survive and grow more than another subclone, the cells of which may die.
The extent to which we’ve been able to analyse the DNA of different subclones within the same tumour has previously been restricted, making it difficult glean information we can use to outwit lung cancer.
But now, thanks to TRACERx, that’s changing.
“Ever-changing ecosystems”
 An example visualisation of a phylogenetic tree. The blue spot (top) would be the trunk of the tree, and the green, orange and dark blue spots are subclones that form from it. The green and orange spots are then selected for, further developing and forming new subclones.</p>
<p>(Bottom) An example visualisation of subclones growing within a tumour.</p>
<p> ” data-medium-file=”https://news.cancerresearchuk.org/wp-content/uploads/2023/04/TRACERx-image-176×300.jpg” data-large-file=”https://news.cancerresearchuk.org/wp-content/uploads/2023/04/TRACERx-image.jpg” decoding=”async” class=” size-medium wp-image-25541″ src=”https://news.cancerresearchuk.org/wp-content/uploads/2023/04/TRACERx-image-176×300.jpg” alt=”An example visualisation of a phylogenetic tree, and of subclones growing within a tumour” width=”176″ height=”300″ srcset=”https://news.cancerresearchuk.org/wp-content/uploads/2023/04/TRACERx-image-176×300.jpg 176w, https://news.cancerresearchuk.org/wp-content/uploads/2023/04/TRACERx-image-150×255.jpg 150w, https://news.cancerresearchuk.org/wp-content/uploads/2023/04/TRACERx-image.jpg 300w” sizes=”(max-width: 176px) 100vw, 176px”></p>
<p class=) (Top) An example visualisation of a phylogenetic tree. The blue spot (top) would be the trunk of the tree, and the green, orange and dark blue spots are subclones that form from it. The green and orange spots are then selected for, further developing and forming new subclones. (Bottom) An example visualisation of subclones growing within a tumour.
(Top) An example visualisation of a phylogenetic tree. The blue spot (top) would be the trunk of the tree, and the green, orange and dark blue spots are subclones that form from it. The green and orange spots are then selected for, further developing and forming new subclones. (Bottom) An example visualisation of subclones growing within a tumour.
In one piece of their newly published research, the TRACERx team took multiple samples from over 400 tumours to try and determine the order that these subclones developed in, and why certain subclones were selected for where others weren’t. Doing that could give us clues as to what a person’s cancer might do next.
“By looking at different pieces of the same tumour, we can trace back how it developed in a particular patient,” says Dr Alexander Frankell, who led this project.
“We’ve done this for more than 400 cancer patients in the TRACERx study, which allowed us to spot common patterns, shedding light on how lung cancers arise in the body but also why some patients have a much worse survival than others.”
For example, they found that mutations called whole genome doubling, where the entire set of genes in the cell doubles, was associated with poorer prognosis.
In addition, chromosomal instability, which is a persistent loss or gain of entire chromosomes from a cell, was associated with a higher likelihood of a cancer coming back within 1 year after it’s been removed by surgery. What’s more, it means the cancer is more likely to spread to other areas beyond the lungs.
Armed with this knowledge, doctors treating people with lung cancer could identify those whose cancer is most at risk of returning after surgery and intervene by following up with further treatment, like chemotherapy, to help prevent it from coming back.
“TRACERx recognises that cancer is not static and the way we treat patients shouldn’t be either,” says Professor Charles Swanton, Cancer Research UK’s chief clinician and lead researcher on TRACERx.
“What makes the TRACERx project particularly powerful is that it treats tumours as ever-changing ecosystems made up of diverse cancer cell populations.
“By looking at the tumour in its entirety, we can observe how these cell populations interact and even compete with one another, gleaning valuable insights into how the tumour is likely to evolve over time, spread and respond to treatment.”
Spotting cells that will spread
When a cancer spreads from where it first started to grow, called the primary tumour, to another area of the body, it’s called metastasis. Metastasis is associated with very poor prognosis and, despite advances in cancer research, has remained incredibly difficult to prevent and treat.
If we’re to prevent metastasis, we need to identify which cells in a tumour are most likely to break away and spread to another part of the body and, most importantly, why.
And to build on their research into the evolution of lung cancer, TRACERx researchers are on the case.
In another of their papers published today, they analysed samples of both primary and metastatic tumours in people whose lung cancer had spread and compared them to regions of lung tumours in people whose cancer hadn’t spread.
From their analysis, they were able to determine that the subclones that were most likely to spread developed later in the tumour’s growth, after an event called a clonal sweep, where one subclone will outgrow the others and become dominant
In addition, in approximately 70% of patients, the metastases were seeded by only one subclone, rather than each metastasis being seeded by a different subclone.
They also were able to identify specific mutations in subclones that made them more likely to metastasise, meaning it would break away from the primary tumour and travel to and grow in a different area of the body.
Developing our understanding of which genetic changes in a tumour could cause metastasis could allow us to develop treatments that target these specific subclones. As metastasis causes the majority of cancer deaths, being better equipped to treat, or even prevent, it could be revolutionary in lung cancer medicine.
The future of TRACERx
This suite of new findings adds to the wealth of knowledge researchers have already uncovered through TRACERx.
In September, we reported on results presented at the European Society for Medical Oncology conference detailing how exposure to air pollution promotes the growth of cells carrying cancer-causing mutations in the lungs. These results were also published in Nature last week.
With the publication of these results, the first phase of TRACERx is coming to a close. But this is by no means the end for TRACERx.
In November, we announced TRACERx EVO, a 7-year programme to build on the groundbreaking discoveries of TRACERx.
Led by an international group of researchers, this new programme has been awarded almost £15 million in funding to continue to transform the field of lung cancer research through data sharing, development of new technologies, and training the future leaders in lung cancer research.
Jacob




