On 15 October 2021, the US Food and Drug Administration (FDA) approved atezolizumab (Tecentriq, Genentech, Inc.) for adjuvant treatment following resection and platinum-based chemotherapy in patients with stage II to IIIA non-small cell lung cancer (NSCLC) whose tumours have PD-L1 expression on ≥1% of tumour cells, as determined by an FDA-approved test.
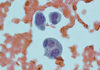
The FDA also approved the VENTANA PD-L1 (SP263) Assay (Ventana Medical Systems, Inc.) as a companion diagnostic device to select patients with NSCLC for adjuvant treatment with Tecentriq.
Efficacy was demonstrated in a multicentre, randomised, open-label study (IMpower010, NCT02486718) in patients with stage IB (tumours ≥4 cm) through stage IIIA NSCLC (per UICC/AJCC staging system, 7th edition). A total of 1005 patients who had complete tumour resection and cisplatin-based adjuvant chemotherapy were randomised (1:1) to receive atezolizumab 1200 mg every 3 weeks for 16 cycles or best supportive care (BSC).
The major efficacy outcome measure was disease-free survival (DFS) as assessed by the investigator in the primary efficacy analysis population (n=476) of patients with stage II-IIIA NSCLC with PD-L1 expression on ≥1% of tumour cells (PD-L1 ≥1% TC). Median DFS was not reached (95% confidence interval [CI] 36.1, NE) in patients in the atezolizumab arm compared with 35.3 months (95% CI 29.0, NE) in the BSC arm (hazard ratio [HR] 0.66; 95% CI 0.50, 0.88; p = 0.004).
In a pre-specified secondary subgroup analysis of patients with PD-L1 TC ≥50% stage II-IIIA NSCLC, the DFS HR was 0.43 (95% CI 0.27, 0.68). In an exploratory subgroup analysis of patients with PD-L1 TC 1-49% stage II-IIIA NSCLC, the DFS HR was 0.87 (95% CI 0.60, 1.26).
The most common (≥10%) adverse reactions in patients receiving atezolizumab, including laboratory abnormalities, were increased aspartate aminotransferase, blood creatinine, and alanine aminotransferase, as well as hyperkalaemia, rash, cough, hypothyroidism, pyrexia, fatigue/asthenia, musculoskeletal pain, peripheral neuropathy, arthralgia, and pruritus.
The recommended atezolizumab dose for this indication is 840 mg every 2 weeks, 1200 mg every 3 weeks, or 1680 mg every 4 weeks for up to 1 year.
Full prescribing information for Tecentriq is available here.
This review was conducted under Project Orbis, an initiative of the FDA’s Oncology Center of Excellence. Project Orbis provides a framework for concurrent submission and review of oncology drugs among international partners. For this review, FDA collaborated with the Australian Therapeutic Goods Administration, the Brazilian Health Regulatory Agency, Health Canada, Switzerland’s Swissmedic, and the United Kingdom’s Medicines and Healthcare products Regulatory Agency. The application reviews are ongoing at the other regulatory agencies.
This review used the Real-Time Oncology Review pilot programme, which streamlined data submission prior to the filing of the entire clinical application, and the Assessment Aid, a voluntary submission from the applicant to facilitate the FDA’s assessment. The FDA approved this application 6 weeks ahead of the FDA goal date.
This application was granted priority review.
Healthcare professionals should report all serious adverse events suspected to be associated with the use of any medicine and device to FDA’s MedWatch Reporting System.
For assistance with single-patient INDs for investigational oncology products, healthcare professionals may contact OCE’s Project Facilitate.