
All of us are impacted by cancer in our lifetime, either facing a diagnosis ourselves or supporting a friend or loved one.
However, a landmark report on deprivation and cancer launched at the Scottish Cancer Conference today shows that the burden of cancer is not felt equally across Scotland.
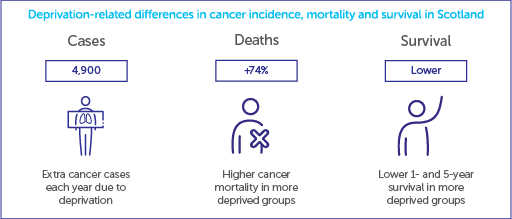
People living in more deprived areas in Scotland are more likely to get cancer and are, sadly, more likely to die from the disease than those in less deprived areas. Cancer death rates are a startling 74% higher in the most deprived populations than the least deprived. The report also estimates that around 4,900 extra cancer cases each year in Scotland are due to deprivation. That’s 13 extra new diagnoses per day that could be avoided if the most deprived areas had the same cancer rates as the least deprived.
The report sets out the urgent need to address inequalities across the cancer pathway, from reducing preventable causes of cancer, to removing barriers to early diagnosis and high-quality treatment, whilst also improving data collection to build a stronger understanding of cancer inequalities in Scotland and what is driving them.
Cancer prevention
Scotland has the highest proportion of cancers caused by preventable risk factors than any other UK nation. Smoking is the biggest cause of cancer in Scotland, responsible for nearly 1 in 5 cases. But we also know that smoking is more common in the most deprived populations. In 2019, 32% of people in the most deprived population smoked, compared to 6% in the least deprived.
The Scottish Government has set a welcomed ‘tobacco-free’ target of less than 5% of adults smoking by 2034. However, based on current trajectories, smoking prevalence for the most deprived may not even reach 10% in the next 25 years. Therefore, without sustained efforts to reduce smoking in the more deprived groups, these groups will experience a higher risk of getting cancer for many decades to come.
 100vw, 512px”></p>
<p class=) Rates of smoking by deprivation for adults. Scotland, 2003-2018, projected to 2040
Rates of smoking by deprivation for adults. Scotland, 2003-2018, projected to 2040
Taken together, overweight and obesity is the second largest preventable cause of cancer in Scotland. Like smoking, obesity rates are higher in more deprived populations. The difference is particularly stark in childhood obesity rates, with children living in more deprived areas twice as likely to live with obesity compared to those in less deprived areas of Scotland. The world around us plays a big part in how easy it is to maintain a healthy weight, which is why population-wide measures, such as those outlined in the Scottish Government’s obesity strategy, are needed.
Cancer diagnosis and treatment
Diagnosing more cancers at an early stage is essential for improving cancer outcomes. But catching cancer early in deprived areas can be more challenging. There are various reasons for this.
There is a large gap in the uptake of cancer screening invitations. For example, for breast and bowel screening, uptake is 20 percentage points lower in the most deprived populations compared to the least deprived. Research also shows that amongst deprived groups, there is reduced awareness of some cancer symptoms and people are more likely to report barriers to seeking help. Another significant bottleneck in the cancer pathway for patients in Scotland lies in diagnostic services, exacerbated by regional variation in specialist workforce capacity.
Given that research shows that people in deprived populations are already more likely to be diagnosed with cancer at advanced stages, measures to improve early diagnosis for everyone in Scotland are vital to improve overall cancer outcomes.
It is also essential that no matter where patients live in Scotland, they have timely access to treatment. Performance against the 62-day standard – which states that at least 95% of eligible patients wait no more than 62 days from an urgent suspected cancer referral to begin treatment – varies greatly between NHS Health Boards; in 2021, performance against the 62-day target ranged between 67% and 94%. The Scottish Government must invest to expand capacity across NHS cancer services including long-term funding for workforce education and training for key cancer specialities.
 100vw, 512px”></p>
<p class=) Screening programme uptake by deprivation, Scotland
Screening programme uptake by deprivation, Scotland
Now is the time to go further and faster
Deprived populations in Scotland face significant barriers to good health which are creating unacceptable inequalities in cancer incidence and outcomes for patients.
Cancer Research UK wants to accelerate progress so that 3 in 4 people survive their cancer for 10 years or more by 2034. We must ensure that improvements in cancer outcomes are experienced by everyone.
Firstly, more evidence is needed to understand cancer and deprivation. Health data collection, infrastructure and access should be strengthened. Data should be routinely collected on patient characteristics, including age, gender, ethnicity, sexuality and deprivation, to improve wider understanding of where inequalities exist and what is driving them.
The Scottish Government must ensure that its next tobacco strategy includes bold measures to reduce smoking and inequalities. We need more government action to ensure young people don’t start smoking, and funding for the measures and services needed to help people quit. That’s why Cancer Research UK has launched its latest Smokefree UK campaign. As part of this, we are calling for a Smokefree Fund, which would make the tobacco industry – not the taxpayer – foot the bill for the harm it causes, but without their influence on how the money is spent. We encourage the Scottish Government to work with the UK Government to make this happen.
The Scottish Government should also fully implement the measures outlined in its obesity strategy, including the forthcoming legislation restricting price promotion offers on unhealthy food and drink.
Additionally, the Scottish Government must implement interventions that reduce inequalities across cancer care, by removing barriers to seeking help and enabling timely access to health services. This should come alongside an investment to increase capacity in cancer services, in particular through ensuring long term funding for workforce expansion. This investment should be particularly targeted to tackle regional variation in the cancer workforce.
Reducing cancer inequalities has been identified as a key goal of the upcoming 10-Year Cancer Strategy in Scotland which is due to be published in early 2023. Our Cancer Research UK volunteer ambassadors have already set out what they would like to see in the Scottish Government’s upcoming strategy. This report illustrates why addressing inequalities must be central to this new strategy, so that it can truly be a cancer plan for all.





