A randomised, non-comparative, multicentre, open-label, phase II PHERGain study showed that an 18F-FDG-PET-based, pathological complete response (pCR)-adapted strategy can identify a group of patients with HER2-positive early breast cancer who can safely omit chemotherapy and receive exclusive dual HER2 blockade with trastuzumab and pertuzumab.
The 3-year invasive disease-free survival (iDFS) rate from surgery for patients in group B treated with this de-escalating approach was 94.8% despite omitting chemotherapy in around one third of patients. Strong 3-year outcomes were observed among group B 18F-FDG-PET–responder patients who obtained a pCR with trastuzumab and pertuzumab and never received chemotherapy without any metastatic relapse. The findings are published by Dr. Antonio Llombart Cussac of the Hospital Arnau de Vilanova, Universidad Católica de Valencia in Valencia, Spain, and colleagues on 3 April 2024 in The Lancet.
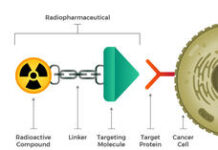
The authors wrote in the background that neoadjuvant setting represents the best scenario for chemotherapy de-escalation, considering that pCR is a well-defined surrogate marker for long-term DFS and overall survival. There is a significant focus on non-invasive imaging tools that monitor the response to preoperative therapy. Among patients with HER2-positive early breast cancer, early metabolic evaluation using 18F-FDG-PET selected HER2-positive tumours with high anti-HER2 sensitivity and an increased likelihood of having a pCR to neoadjuvant HER2 blockade.
PHERGain is an international, randomised, open-label, phase II study that evaluated the feasibility of a chemotherapy-free strategy based on a dual HER2 blockade with trastuzumab and pertuzumab plus endocrine therapy for hormone receptor-positive tumours in patients with HER2-positive early breast cancer through an 18F-FDG-PET-based, pCR-adapted strategy.
At the first planned analysis, the study met its first primary endpoint. A total of 227 of 285 patients (80%) in group B, who were treated exclusively with a dual HER2 blockade of trastuzumab and pertuzumab without chemotherapy, were 18F-FDG-PET responders. From this group of 18F-FDG-PET responders, 86 patients (38%) reached a pCR (95% confidence interval [CI] 31.6–44.5]; p < 0.0001 compared with the historical rate).
In the latest article published in The Lancet, the authors report the results for the second primary endpoint, 3-year iDFS among patients included in group B who underwent surgery according to protocol. Additional efficacy endpoints and updated safety results from groups A and B are also reported.
PHERGain took place in 45 hospitals in seven European countries. It randomly allocated patients in a 1:4 ratio with centrally confirmed, HER2-positive, stage I–IIIA invasive, operable breast cancer with at least one PET-evaluable lesion to either group A, where patients received docetaxel, carboplatin, trastuzumab, and pertuzumab, or group B, where patients received trastuzumab and pertuzumab with or without endocrine therapy, every 3 weeks. Random allocation was stratified by hormone receptor status. Centrally reviewed PET was conducted at baseline and after two treatment cycles.
Patients in group B were treated according to on-treatment PET results. Patients in group B who were PET-responders continued with trastuzumab and pertuzumab with or without endocrine therapy for six cycles, while PET-non-responders were switched to receive six cycles of docetaxel, carboplatin, trastuzumab, and pertuzumab. After surgery, patients in group B who were PET-responders who did not achieve a pCR received six cycles of docetaxel, carboplatin, trastuzumab, and pertuzumab, and all patients completed up to 18 cycles of trastuzumab and pertuzumab.
Between 26 June 2017 and 24 April 2019, a total of 356 patients were randomly allocated, 71 patients in group A and 285 patients in group B, and 63 (89%) and 267 (94%) patients proceeded to surgery in groups A and B, respectively. At this second analysis with data cut-off on 4 November 2022, the median duration of follow-up was 43.3 months (range, 0-63). In group B, the 3-year iDFS rate was 94.8% (95% CI 91.4–97.1; p = 0.001), meeting the primary endpoint.
No new safety signals were identified. Treatment-related adverse events and serious adverse events (SAEs) were numerically higher in patients allocated to group A than to group B with grade ≥ 3 62% versus 33% and SAEs 28% versus 14%. Group B PET-responders with pCR presented the lowest incidence of treatment-related grade 3 or higher adverse events (1%) without any SAEs.
The authors concluded that among patients with HER2-positive early breast cancer, a PET-based, pCR-adapted strategy was associated with an excellent 3-year iDFS. This strategy identified about a third of patients who had HER2-positive early breast cancer who could safely omit chemotherapy. Although such a strategy will require further clinical investigation and prolonged follow-up, the study offers a new therapeutic alternative to be considered in clinical practice that enables a significant reduction of toxicity for this patient population without compromising efficacy.
In an accompanied comment, Dr. Helena M Earl of the Department of Oncology, University of Cambridge in Cambridge, UK wrote that PHERGain study successfully optimised, and thereby personalised and de-escalated, treatment while preserving the same long-term outcomes for patients. In terms of further prospect in the field, the investigators are already working on algorithms which will include molecular signatures in HER2-positive disease, refined imaging biomarkers, and liquid biopsies for circulating tumour DNA, alongside conventional clinical and pathological features. Using artificial intelligence and machine learning, more sensitive and specific predictors of pCR could be developed and validated, allowing safe and convenient de-escalation of chemotherapy for a more precisely defined group of patients with early HER2-positive breast cancers.
F Hoffmann-La Roche funded the study and provided trastuzumab and pertuzumab for the study.