Cancer Grand Challenges is a global funding initiative co-founded by Cancer Research UK and the National Cancer Institute (NCI) in the US.
Recognising the need for team science to drive us forward, Cancer Grand Challenges provides up to £20 million in funding to diverse, global research teams, giving them the freedom to come together, think differently and take on some of the most complex challenges in cancer research.
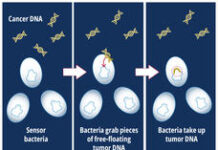
These teams utilise the power of unprecedented multidisciplinary collaboration to find bold solutions to challenges that continue to stand in the way of progress in cancer research – from distinguishing between lethal and non-lethal cancers to uncovering how microbes in our body affect cancer treatment.
7 teams across 9 countries have each received funding so far, and today, Cancer Grand Challenges announced four new teams that have each received £20 million in funding to take on the biggest challenges in cancer research, set by their expert scientific committee.
So, what are the challenges that the new teams are working on? And what makes them grand challenges?
In part 1 of Inside Cancer Grand Challenges, we’ve dived into two of them with the help of Professor Charles Swanton, our chief clinician and member of the Cancer Grand Challenges scientific committee.
Improving quality of life
Up to 8 in 10 patients with advanced cancers will experience severe weight loss, losing both fat and muscle, due to a wasting syndrome called cachexia.
Cachexia is very different to general weight loss. It is an irreversible condition, and continues even when the person is able to eat normally or fed through a tube.
The weight loss characteristic of cachexia is often accompanied by fatigue, broad organ and tissue dysfunction, and a greatly diminished quality of life. To make matters worse, cachexia limits a person’s ability to receive systemic therapies for their cancer, which results in a poor prognosis.
But despite major clinical implications, relatively little is known about what causes cachexia, or how to effectively treat it. That’s where one of the newly funded Cancer Grand Challenges teams, the Cancer Cachexia Action Network (CANCAN), comes in.
“Cachexia is one of the biggest problems we deal with in solid-tumour oncology, and advances in care will come with a deeper understanding of the mechanisms involved,” says Swanton.
“If we can intervene in that pathway, we’ll be perfectly placed to start to improve the health and wellbeing of our patients, which I hope will help to improve the efficacy of therapy.”
The Cachexia challenge seeks to expand our understanding of the mechanisms of cachexia and fatigue that severely impact the quality of life of people with cancer and limits their therapeutic options.
CANCAN brings together a diverse group of scientists from a wide range of fields, from immunologists to experts in metabolic diseases and neuroendocrine function, to discover what drives cachexia on a molecular level.
Co-led by cancer biologist Eileen White, physician scientist Marcus DaSilva Goncalves, and biochemist and medical oncologist Tobias Janowitz, the team’s range of specialisms aims to overcome the barriers individual groups face trying to investigate cachexia alone.
“Understanding that complex relationship between the tumour and the body is going to be key to really deciphering this this problem,” says Swanton. “And that’s why this grand challenge, I think, is so important.”
Finding effective treatments for children
Cancer remains a leading cause of death by disease in children worldwide.
Whilst survival for some paediatric cancers, like blood cancers, has improved, survival for solid tumours hasn’t improved in over three decades.
Current therapies for treating solid tumour cancers in children are limited, and standard treatments like radiotherapy and chemotherapy can have life-long side effects, from abnormal growth to infertility.
The Solid Tumours in Children challenge aims to develop new therapies for these tumours, and help more children survive them.
Co-led by physician scientists Catherine Bollard in the US and Martin Pule in the UK, the NexTGen team hopes to produce effective CAR T-cell therapy, a type of immunotherapy, for children with sarcomas and brain tumours.
The team comprises experts in oncology, immunology, glycobiology, proteomics and mathematics, with extensive experience in translating scientific discoveries to clinical settings.
They aim to bring CAR T-cell therapies to the front line of therapies for children within the next decade.
“CAR T-cell therapies have had incredible success in the context of childhood leukaemia, but their progress in solid tumours has been relatively slow,” says Swanton. “And this Cancer Grand Challenge is primed to really accelerate progress in this in this key area of unmet need in paediatric oncology.
“And this is something that really is only possible through Cancer Grand Challenges, because these are relatively low incidence tumours, these aren’t tumours that traditionally are targeted by the pharma industry.
“We’ve got all the tools now; we know what to do. Now what we need to do is bring research groups together across the world to be able to enable and deliver these therapies for the benefits of children.”
Making a positive impact
The impact that demystifying cachexia and uncovering new therapies for children could have on cancer care is immense, and these are just 2 of the 10 challenges currently being tackled by the Cancer Grand Challenges community.
Whilst we have been supporting this community since 2017, this is the first round of teams under the new partnership with the NCI.
The partnership has taken the initiative to a whole new scale, increasing the scope, depth and breadth of research that can be undertaken. Together with the NCI, we will co-fund up to 12 teams over 3 rounds of funding, including the 4 announced today.
“I am fortunate to work as both a scientist and clinician and am very excited about the future clinical impact of these Cancer Grand Challenges,” says Swanton.
“I know there is an urgent need for new cancer treatments for children. I’ve also seen first-hand the extreme weight loss and lethargy that patients experience from cancer cachexia and the need to develop treatments to combat this clinical challenge that is associated with poor outcomes.
“That’s why I am so excited that we are funding these challenges because they have the potential to have a profound and positive impact for patients.”
Jacob
- Inside Cancer Grand Challenges Part 1: what makes a grand challenge?