, by NCI Staff
Results from a large study are expected to help determine the best treatment approach for some people with an advanced form of melanoma.
The NCI-sponsored clinical trial, called DREAMseq, included people with metastatic melanoma whose tumors had a specific mutation in the BRAF gene, called V600. It tested initially giving patients a combination of the immunotherapy drugs ipilimumab (Yervoy) and nivolumab (Opdivo) or a combination of the targeted therapies dabrafenib (Tafinlar) and trametinib (Mekinist). In both patient groups, once the initial treatment was no longer working, they were switched to the other treatment combination.
More of the patients treated first with immunotherapy drugs were alive at 2 years compared to patients treated first with the targeted therapy combination (72% versus 52%). The difference was substantial enough that the trial was stopped early by its data safety and monitoring board.
Both drug combinations have been found to be effective in people with advanced melanoma. But for the estimated 50% of people whose melanomas have a BRAF V600 mutation, researchers didn’t know which treatment combination was better to use first. For these patients, there now appears to be an answer.
According to Michael Atkins, M.D., of the Georgetown Lombardi Comprehensive Cancer Center, who led the trial, the findings support an immediate change in clinical practice and will have “a significant impact on clinical care.” Dr. Atkins presented results from the trial as part of the American Society of Clinical Oncology Virtual Plenary Series on November 16.
“The results are spectacular,” said Elad Sharon, M.D., who helps lead immunotherapy trials in NCI’s Cancer Therapy Evaluation Program but was not involved in the DREAMseq trial. “Not only were the results impressive enough that you can see a difference between the [treatments]—you saw so much of a difference that they were able to stop the trial early.”
Checkpoint inhibitors versus BRAF-targeted therapies
When caught early, melanoma is curable, often with surgery alone. But if the cancer spreads, or metastasizes, it’s much more difficult to treat.
However, substantial progress has been made in the treatment of metastatic melanoma over the last decade, including the discovery of cancer-fueling BRAF mutations and the development of therapies that target tumors with these mutations.
Dabrafenib, which blocks the activity of V600-mutated BRAF proteins, was first approved by the Food and Drug Administration (FDA) in 2013 as a standalone treatment for advanced melanoma with certain mutations in the BRAF gene, and the combination of dabrafenib and trametinib was approved in 2014.
Trametinib inhibits the activity of a different protein, called MEK, that often works in conjunction with BRAF. It is also approved for advanced melanoma that has certain BRAF mutations. Dabrafenib and trametinib are both taken as pills.
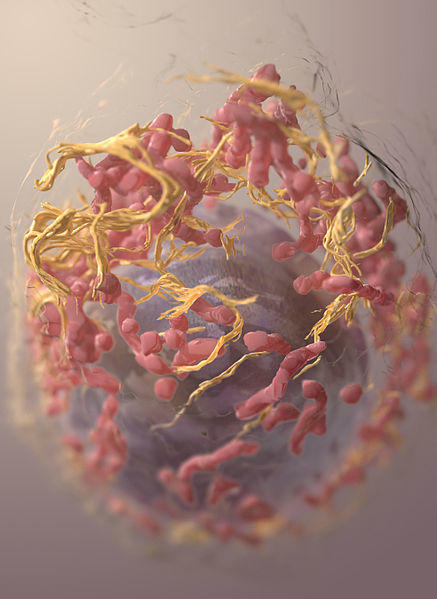
Soon after these targeted therapies were developed, a new category of drugs called immune checkpoint inhibitors rapidly emerged as effective treatments for melanoma. These drugs block proteins on cancer cells or immune cells called immune checkpoints. Blocking immune checkpoint proteins helps immune cells find and kill cancer cells.
Both ipilimumab and nivolumab were initially approved as standalone treatments for patients with metastatic melanoma. In 2016, they were approved in combination to treat people with metastatic melanoma, regardless of whether their tumors had BRAF mutations. Ipilimumab and nivolumab are administered intravenously.
Before the DREAMseq trial, a key consideration in choosing which class of drugs to use as an initial treatment was their side effects.
“The side effects of these two types of therapy are completely different,” Dr. Atkins explained. Because the BRAF mutation only occurs in the tumor, targeted therapies specifically target tumor cells and generally cause fewer effects in healthy cells. Although the dabrafenib–trametinib combination does cause side effects—most commonly fatigue, fever, joint problems, and nausea—they don’t tend to be life-threatening.
Immunotherapy drugs like nivolumab and ipilimumab can cause “the immune system to get overactivated” and attack a patient’s healthy tissues, Dr. Atkins said. These side effects are often more severe and involve a variety of organs.
The combination of nivolumab and ipilimumab can sometimes permanently damage normal organs, like the thyroid gland or the pituitary gland, he continued. People with these side effects may have to take hormone replacement therapy for the rest of their lives.
Because the side effects of immune checkpoint inhibitors tended to be more severe than those caused by targeted therapies, “for many people, it was easier to consider using the BRAF-targeted drugs if the [patient’s tumor] had a BRAF mutation,” Dr. Sharon said. However, no study had compared the two treatment regimens directly.
“We had these two new effective treatment strategies for patients with advanced BRAF+ melanoma,” Dr. Atkins summarized. “And the question was, which of these approaches is better? And given that patients would have access to both of these approaches, is there a particular sequence of those two approaches that lead to the best outcome?”
Results from the DREAMseq trial
The DREAMseq trial, which was led by the ECOG-ACRIN research group, included 265 people with metastatic melanoma whose tumors had BRAF V600 mutations.
The trial was sponsored by NCI, but also included funding from Bristol Meyers Squibb (the manufacturer of ipilimumab and nivolumab) and Novartis Pharmaceuticals (the manufacturer of dabrafenib and trametinib). About 14% of patients had already received some form of postsurgical (adjuvant) treatment for melanoma when they joined the trial.
First, patients were randomly assigned to receive either combination immunotherapy (ipilimumab plus nivolumab) or combination targeted therapy (dabrafenib plus trametinib).
If a patient’s cancer was resistant to initial treatment and progressed, or initially responded to treatment only to return later, they received the second treatment option. Patients who had initially received immunotherapy switched to the targeted therapy combination, and those who had started with the targeted therapies switched to the immunotherapy combination.
Overall, 73 people moved on to the second treatment option: 27 who first received immunotherapy and 46 who first received targeted therapies.
More than half of people (63%) who did not switch to a second drug option did so because their cancers did not progress, so they stuck with the therapy they were initially assigned. The rest did experience disease progression but either died before they could begin the second therapy option or did not move on for other reasons.
Before enough time had passed for more patients to begin treatment with a second drug due to disease progression, the trial was stopped early by the data safety monitoring board.
After reviewing data from the first 265 patients, the safety board found that 72% of patients who were initially treated with the immunotherapy combination—whether or not they went on to receive the targeted therapy combination—were still alive 2 years after starting treatment. Among those initially treated with targeted therapies, 52% were still alive after 2 years.
When the trial was stopped, participants who were still receiving initial treatment with the targeted therapies were immediately given the option to switch to the ipilimumab–nivolumab combination.
“I think [standard of care] should immediately change because these are FDA-approved regimens,” said Dr. Atkins. “[Physicians] seeing these results should consider patients who are on initial targeted therapy for a switch to immunotherapy.”
Most patients who participated in the trial experienced serious side effects. Overall, however, serious side effects occurred most often in patients who received immunotherapy as their initial treatment.
| Treatment group | First-line serious side effects | Second-line serious side effects |
| Immunotherapy | 60% | 52% |
| Targeted therapy | 54% | 50% |
Three people died as a result of treatment. Two people who had been treated only with combination immunotherapy died: one from an inflammatory heart condition called myocarditis and one from gastrointestinal side effects. One person died as the result of a stroke while being treated with second-line targeted therapy.
Patients with BRAF+ advanced melanoma “should first receive an immunotherapy combination,” Dr. Sharon agreed. “You would have to have some significant reason why the [targeted therapy] combination would be better for a particular patient.”
Nonetheless, he acknowledged, “there is probably a higher risk of fatal side effects associated with immunotherapy treatments, and that is something patients have to be aware of.”
Following up on a practice-changing result
While the path ahead for these specific treatment options seems clear, there are some questions that DREAMseq is unable to answer.
The results from the trial show that, in general, initial immunotherapy results in better overall survival for people with advanced BRAF+ melanoma. However, for a small proportion of patients, targeted therapies seemed to prevent death shortly after beginning treatment (often called early death) better than immunotherapies. Researchers are working on “identifying markers for who’s going to respond best to particular therapies,” Dr. Atkins explained.
Because DREAMseq only tested two specific drug combinations, it’s not clear whether other available therapies alone, or different combinations of therapies, may produce better results.
Also, newer therapies have been developed that were not tested in this trial. For example, in 2020, FDA approved atezolizumab (Tecentriq), another immune checkpoint inhibitor, for use in combination with the targeted BRAF inhibitors cobimetinib (Cotellic) and vemurafenib (Zelboraf) to treat BRAF+ melanoma.
That approval happened while DREAMseq was underway, so a trio of atezolizumab and BRAF/MEK inhibitors has not been compared with the immunotherapy combination in a clinical trial.