Gliomas are a type of brain tumour that originate in cells called glial cells.
As with most brain tumours, surgery is the most common treatment option for gliomas. But brain surgery is understandably invasive, and can’t always remove the whole tumour, meaning it often has to be followed up with other treatments.
If we can find a way to successfully treat brain tumours with therapies like chemotherapy, we can make treatment kinder for patients.
However, treating brain tumours with chemotherapy proves more difficult than for other tumours. In fact, most chemotherapies can’t be used on brain tumours at all because the drugs can’t get into the brain. That’s down to what’s called the blood-brain barrier.
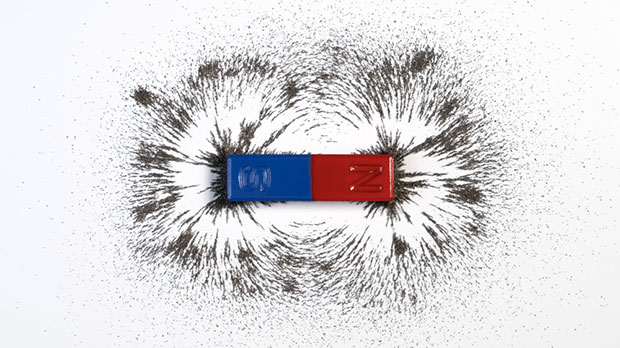
The blood-brain barrier acts as a kind of security check for brain cells.
Oxygen, nutrients, and other things circulating in our blood that brain cells need to survive are allowed to pass through the barrier, whereas a complex network of physical barriers and metabolic hurdles like enzymes block out everything else.
Its purpose is to protect brain cells from anything that might harm them, like bacteria or viruses you might have in your blood if you’re unwell. But that creates a problem for chemotherapy. If the drug can’t get through the barrier, it can’t treat a tumour.
There are chemotherapies that can penetrate the barrier, but very few, meaning that invasive surgery remains the primary treatment for brain tumours.
So, to make it a more useable treatment, we need to find a way to give chemotherapy a helping hand in getting through this barrier into the brain.
And we’ve found one: a magnet.
A futuristic treatment?
Using magnets to deliver treatments to a specific site in the body might sound futuristic, but the idea was first proposed back in the 1960s and considered in the context of cancer treatment by the late 1970s.
To do it, you attach a drug to a tiny particle called a magnetic nanoparticle (MNP) and then use a magnet to direct those particles to a particular site in the body.
For example, if you bind MNPs to a chemotherapy drug, give that drug to a patient intravenously and create a magnetic field around a particular organ, the blood circulation will carry the MNPs through the body until they reach that organ, where they’ll ‘stick’ due to the attraction of the MNPs to the magnetic field.
The advantage of delivering drugs like this is that it ensures the delivery of the drug is focussed to the correct place in the body, ensuring that the maximum amount of the drug reaches the tumour whilst minimising off-target effects.
And there have even been a few early phase clinical trials using this technique, which is called magnetic drug targeting.
The results of these trials have been promising but were done in people with cancers where the tumour is relatively close to the surface of the body, like liver cancer.
Brain tumours are a trickier problem because they’re deeper in the body, which makes it difficult for magnetic fields to penetrate to the tumour.
So, we need stronger magnets, like the ones used in an MRI scanner, to create a stronger magnetic field.
This has been trialled before too, to similar degrees of success, but as anyone who’s ever had an MRI will know, MRI scanners are bulky, noisy and can be uncomfortable. As such, it isn’t a suitable option for people who need regular chemotherapy sessions that can last hours at a time.
So, what do you do when magnetic drug targeting could be a viable treatment option, but current magnetic devices aren’t appropriate for the task?
You design a new one.
Ultimately, our goal is to make the delivery of these sorts of treatments less invasive.
Dr Faith Howard
A magnetic helmet
That’s exactly what a team of researchers at the University of Sheffield, part funded by us, have done.
But while they were thinking big, they had to start small.
They designed a device for mice with brain tumours using magnets called neodymium magnets. These magnets were stronger than the ones used in previous trials, but much smaller and more portable than MRI magnets.
They built these magnets into a kind of helmet, which kept it in the correct position for the course of the treatment and encased them in a way that created a more focussed and stable magnetic field.
They then intravenously administered MNPs made of iron oxide to the mice and put these helmets on them for 30 minutes. After that time, they found that not only had the MNPs made it into the brain successfully, but they were also concentrated in the tumour. That meant the magnet was doing its job.
Once they’d confirmed that, they could put it to the real test.
They attached the same MNPs to a chemotherapy drug called temozolomide, one of the few currently available chemotherapies for brain tumours. They then administered it to the mice intravenously three times over the course of four days and put the helmet on them each time.
“We looked to see how successful the drug delivery was, whether it had actually gone directly to the tumour or spread across the whole brain,” says Dr Munitta Muthana, who leads the research team. “Then we could look to see whether it improved survival and reduced tumour burden.
“And we were really excited by the data.”
The results showed that the magnetised temozolomide significantly reduced the size of the mice’s tumours and extended their survival. Importantly, these mice survived for longer than those who had temozolomide by itself, showing that the magnet made the same dose of drug more effective against the tumour.
What’s more, they didn’t find any MNPs in the liver, spleen or lungs of any of the mice, which tells us that the body can safely break them down and excrete them without any damage to other organs.
Scaling up
This study represents a proof of concept: this small, portable device can successfully concentrate magnetised chemotherapy inside a brain tumour. But what’s even more exciting is the possibilities that could lead to.
“We didn’t want this to be about temozolomide because we already use that to treat patients with brain tumours. There are so many other chemotherapies and other drugs out there that aren’t given to these patients,” says Muthana.
“So next steps will be to replace that drug with drugs that perhaps wouldn’t currently be used for this purpose.”
If we can help other drugs to cross the blood-brain barrier using these magnets, there’s the opportunity to greatly increase the number of drugs we have available to treat brain tumours.
“Ultimately, our goal is to make the delivery of these sorts of treatments less invasive,” adds Dr Faith Howard, a Cancer Research UK-funded postdoctoral research associate in the team.
“The way we treat gliomas is to directly inject chemotherapies into the brain, which is a very invasive, risky surgery and it can only be performed a limited number of times. Whereas with a delivery system like this there’s the potential for multiple administrations over a certain period, more drug options, better patient recovery and less time in hospital.”
Though the results are promising, Muthana says we aren’t quite ready to make the jump to using this device to improve treatment in humans. We’ll have to test the treatment out on a bigger animal with a similarly sized brain to us.
But to make sure we’re ready when we do get to humans, they’ve already shown that this magnetic device can be scaled up to human size.
These scaled up magnets are strong enough to penetrate roughly 10 centimetres into the brain. That would allow us to target even very deep tumours, while the portability of the device would allow patients some freedom during treatment.
“We got some brain cancer patients to come in and try on some helmets housing this magnet,” Muthana says. “We got them to make a cup of tea to see what it would feel like, and we’d ask them for feedback about the type of helmets we should make.”
While we may not be seeing it in action in the near future, magnetic drug delivery has the potential to change the face of brain tumour treatment. More patients could be spared invasive surgery, and offered kinder, more flexible treatment.
Jacob
You can read more about Dr Muthana and her group’s research here
 100vw, 138px”></p>
<p class=) Dr Faith Howard
Dr Faith Howard
Dr Faith Howard is a postdoctoral researcher at the University of Sheffield where her work on magnetically guided cancer killing viruses won the BACR Roger Griffin Prize for Cancer Drug Discovery. She has previously worked in the biotech industry for the development of novel vaccines and contract research in the AMR field. Currently, Dr Howard’s areas of interest are nanocarriers to improve targeted drug delivery to hard to reach and advanced cancers.




