December 14, 2018, by NCI Staff
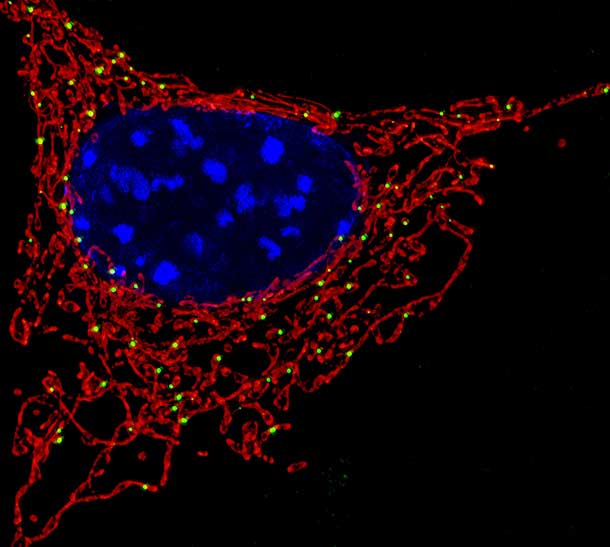
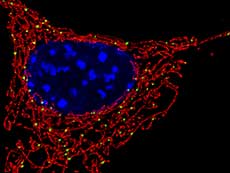
In cells, metabolism takes place in the mitochondria (red).
Credit: National Institute of Child Health and Human Development
Two recent NCI-funded studies may explain why the combination of two cancer therapies is effective against acute myeloid leukemia (AML). The drugs work together to target cancer stem cells, a subset of cells that are thought to give rise to all other cancer cells.
Specifically, the studies showed, the drugs venetoclax (Venclexta) and azacitidine (Vidaza) team up to block the unique metabolism of leukemia stem cells.
Cancer stem cells possess two key properties: the indefinite ability to make copies of themselves, and the ability to give rise to other variations of cancer cells. Because of these characteristics, these specialized cells are thought to be mainly responsible for the initiation, growth, spread, and recurrence of cancer.
Treatments that don’t kill cancer stem cells are like “pulling a weed and not getting the root,” explained lead investigator Craig Jordan, Ph.D., of the University of Colorado School of Medicine. “Of course it is going to come back,” he said. Dr. Jordan and his team, among other researchers, are studying ways to target cancer stem cells.
“If you want to target cancer stem cells specifically, you have to find their unique properties,” said Steven Hou, Ph.D., head of NCI’s Stem Cell Regulation and Animal Aging Section, who was not involved in the studies.
One characteristic that sets cancer stem cells apart is their metabolism—that is, the way they use fuel to create energy. In recent years, researchers have found that cancer stem cells from multiple tumor types rely on one kind of metabolism, called oxidative phosphorylation, more than any other method.
Using samples of cells from people with AML who were treated with the venetoclax–azacitidine combination as part of a clinical trial, Dr. Jordan and his colleagues discovered that the treatment cut off the leukemia stem cells’ fuel for oxidative phosphorylation.
These findings show “for the first time that a therapeutic intervention can eradicate [leukemia stem cells] in patients with AML by disrupting … energy metabolism,” the researchers wrote.
Cancer Stem Cell Metabolism
Leukemia cells rely on a protein called BCL-2 for survival. In previous laboratory experiments, Dr. Jordan and his team discovered that blocking BCL-2 killed leukemia stem cells by interfering with oxidative phosphorylation.
And in an early-phase clinical trial, azacitidine plus venetoclax—a drug that inhibits BCL-2—eliminated all traces of disease in 73% of elderly patients with newly diagnosed AML. Some patients were still responding to the treatment more than a year later.
The frequency and durability of these responses are “remarkably impressive,” said Ravi Majeti, M.D., Ph.D., a leukemia expert at Stanford University who was not involved in these studies.
Dr. Jordan and his colleagues had a hunch that the effectiveness of the experimental treatment might reflect its ability to target leukemia stem cells.
In one of the new studies, published November 12 in Nature Medicine, the researchers examined samples of AML cells from 33 participants of the aforementioned clinical trial. As a control, they also examined the responses of 88 people with AML to other therapies, such as standard chemotherapy. Among these patients, 85% in the venetoclax plus azacitidine group and 51% in the control group had a complete response.
They found that the combination treatment, but not chemotherapy, disrupted oxidative phosphorylation and rapidly killed leukemia stem cells. The researchers distinguished leukemia stem cells from regular leukemia cells by the presence or absence of certain molecules. The combination treatment also killed regular leukemia cells, but not healthy blood stem cells.
From laboratory experiments, the researchers found that only the combination of venetoclax and azacitidine disrupted oxidative phosphorylation and killed leukemia stem cells; neither drug on its own had the same effects.
Cutting Off the Fuel Source
In the companion study, published November 12 in Cancer Cell, Dr. Jordan and his colleagues investigated the metabolism of leukemia stem cells in greater detail.
Using leukemia stem cell samples from three participants of the venetoclax clinical trial, the team found that the combination treatment depleted amino acids, molecules that can be used as fuel for energy metabolism.
Follow-up studies of cancer cells isolated from people newly diagnosed with AML revealed that these leukemia stem cells depended exclusively on amino acids as fuel for oxidative phosphorylation. In the absence of amino acids, the leukemia stem cells were unable to switch to other methods of metabolism or sources of fuel, the researchers found.
By contrast, amino acid deprivation did not greatly affect the growth and survival of healthy blood stem cells and regular cancer cells from the same patients.
These findings suggest that leukemia stem cells from newly diagnosed AML are less “metabolically flexible” than other cells, Dr. Jordan explained. Because they cannot adapt when their preferred fuel source is cut off, the cells die.
But leukemia stem cells from other patients with AML could be different from those in this study, Dr. Hou noted. Variation, or heterogeneity, in the make-up of cancer cells might mean that some people’s leukemia stem cells can switch to other metabolic methods and survive the treatment, he explained.
Leukemia Stem Cells after Relapse
Although venetoclax plus azacitidine seems to be effective for older people with AML who have not received prior treatment for their cancer, other clinical trials have shown that this combination is not very active in people with AML that has come back (relapsed) or did not respond to previous treatment (refractory).
Dr. Jordan’s team reasoned that the metabolism of leukemia stem cells in these patients may be different, such that they are no longer vulnerable to the effects of venetoclax and azacitidine.
Indeed, treatment with venetoclax plus azacitidine did not kill leukemia stem cells from patients with relapsed disease, they found. And, compared with leukemia stem cells from previously untreated patients, those from relapsed patients were less dependent on amino acids and oxidative phosphorylation because they could also metabolize another fuel source: fatty acids.
“In the majority of newly diagnosed AML, [cancer stem cells] are metabolically inflexible—it’s amino acids or nothing,” Dr. Jordan explained. “When the disease progresses, and patients relapse after therapy, the [cancer stem cells] become more flexible. At that point, they can burn other fuels and it’s harder to kill them.”
However, when the researchers treated leukemia stem cells from patients with relapsed disease with venetoclax, azacitidine, and a drug that blocks the intake of fatty acids, the cells died. This triple drug combination may be a potential treatment approach for people with relapsed AML, the researchers wrote.
A Novel Treatment Concept
The unique metabolism of leukemia stem cells is a vulnerability that had not been appreciated as a therapeutic opportunity before, Dr. Jordan said. “We think this is a step in the right direction” toward developing more effective therapies for AML, he added.
And because cancer stem cells from solid tumors such as brain, breast, and pancreatic cancer also rely on oxidative phosphorylation, it might be possible to target them in the same way.
“We hope that scientists who study other cancer types will take that concept and see if its valid for other patients,” said Dr. Jordan.
But it’s not quite clear whether this metabolic vulnerability is the main reason why venetoclax plus azacitidine treatment kills leukemia stem cells, cautioned Dr. Majeti. As an inhibitor of BCL-2, venetoclax was developed to activate a mechanism of cell death called apoptosis.
Whether the predominant effect of venetoclax is through apoptosis or metabolism, “the jury is still out on that,” said Dr. Majeti.