In patients with high-volume and high-risk/low-risk metastatic hormone-sensitive prostate cancer, treatment intensification with darolutamide, androgen deprivation therapy (ADT), and docetaxel increased overall survival (OS), consistent with the overall population; the results in the low-volume subgroup were suggestive of survival benefit. The favourable safety profile of darolutamide was confirmed in the disease volume and risk subgroups. Efficacy and safety outcomes from ARASENS in patients with metastatic hormone-sensitive prostate cancer by disease volume and disease risk are published on 16 February 2023 in the Journal of Clinical Oncology along simultaneous presentation at ASCO 2023 Genitourinary Cancers Symposium in San Francisco, CA, US by Dr. Maha Hussain of the Robert H. Lurie Comprehensive Cancer Center, Northwestern University, Feinberg School of Medicine in Chicago, IL, US and colleagues.
In patients with metastatic hormone-sensitive prostate cancer, early treatment intensification with a combination of ADT plus either docetaxel or an androgen receptor pathway inhibitor (ARPI) improved survival versus ADT alone in several randomised controlled studies. The combination of ADT, docetaxel, and an ARPI was evaluated in several phase III trials (PEACE-1, ENZAMET, and ARASENS). In ARASENS, patients with metastatic hormone-sensitive prostate cancer were randomly assigned to double-blind treatment with either darolutamide or placebo, in combination with ADT and docetaxel. The darolutamide group had a significant reduction in the risk of death by 32.5% (hazard ratio [HR] 0.68; 95% confidence interval [CI] 0.57 to 0.80; p < 0.0001) compared with the placebo group.
Timing of metastatic presentation and disease volume and risk have been used to assess prognosis in patients with metastatic hormone-sensitive prostate cancer. The presence of metastatic disease at initial diagnosis (de novo or synchronous disease) is associated with poorer outcomes compared with developing metastases after local therapy (recurrent or metachronous disease). Disease burden has been defined on the basis of volume of metastases as described in the CHAARTED study. In the LATITUDE study, a benefit of adding an ARPI to ADT was demonstrated in patients with high-risk metastatic hormone-sensitive prostate cancer on the basis of factors associated with poor prognosis, including metastatic burden and Gleason score.
In ARASENS, the treatment effect of darolutamide on OS was favourable in patients with de novo (HR 0.71; 95% CI 0.59 to 0.85) and recurrent (HR 0.61; 95% CI 0.35 to 1.05) metastatic hormone-sensitive prostate cancer. When ARASENS was designed, the final analysis of CHAARTED had not been reported nor had data from LATITUDE been reported. Subgroups on the basis of volume and risk categorisations were not prespecified in ARASENS. The study team conducted these subgroup analyses post hoc to determine if specific subgroups of patients by disease volume or risk would achieve greater benefit from the combination of darolutamide, ADT, and docetaxel.
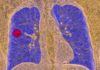
In ARASENS, high-volume disease was defined as visceral metastases and/or ≥ 4 bone metastases with ≥ 1 beyond the vertebral column/pelvis. High-risk disease was defined as ≥ 2 risk factors: Gleason score ≥ 8, ≥ 3 bone lesions, and presence of measurable visceral metastases.
Of 1,305 patients, 1,005 (77%) had high-volume disease and 912 (70%) had high-risk disease. Darolutamide increased OS versus placebo in patients with high-volume (HR 0.69; 95% CI 0.57 to 0.82), high-risk (HR 0.71; 95% CI 0.58 to 0.86), and low-risk disease (HR 0.62; 95% CI 0.42 to 0.90), and in the smaller low-volume subgroup, the results were also suggestive of survival benefit (HR 0.68; 95% CI 0.41 to 1.13). Darolutamide improved clinically relevant secondary endpoints of time to castration-resistant prostate cancer and subsequent systemic antineoplastic therapy versus placebo in all disease volume and risk subgroups.
Adverse events were similar between treatment groups across subgroups. Grade 3 or 4 adverse events occurred in 64.9% of patients treated with darolutamide versus 64.2% in placebo group in the high-volume subgroup and 70.1% versus 61.1% in the low-volume subgroup. Among the most common adverse events, many were known side-effects related to docetaxel.
These subgroup analyses of ARASENS showed that darolutamide plus ADT and docetaxel improves OS in high-volume and high- and low-risk patients with HRs consistent across all subgroups and similar to the overall population. Darolutamide did not increase the toxicity associated with ADT and docetaxel in disease volume and risk subgroups.
The authors commented that the results of ARASENS indicate an advantage to adding darolutamide to ADT and docetaxel, but other studies have shown that benefits are not consistent for all types of ARPIs. Given the unique structure, benefit-risk profile, and limited drug-drug interactions of darolutamide, the results of ARASENS should not be extrapolated to other second-generation ARPIs.
ARASENS was not designed to compare outcomes for triplet combination therapy versus darolutamide plus ADT to evaluate whether docetaxel has added benefit in patients with metastatic hormone-sensitive prostate cancer. In patients with low-volume disease, an additional study evaluating the effect of a triplet combination versus combination with ADT and ARPI might provide more information for optimal treatment selection.
The study was supported by Bayer AG and Orion Pharma.