, by NCI Staff
Immune checkpoint inhibitors work well, and even cure, some people with advanced cancer. But for most patients, these immunotherapies work only for a short time or not at all. Now researchers have evidence that cholesterol-lowering drugs might offer a way to improve those success rates.
In studies of mice, two cholesterol-lowering drugs slowed the growth of tumors on their own and when combined with an immune checkpoint inhibitor, a team from Duke University has found. Both drugs, evolocumab (Repatha) and alirocumab (Praluent), are used to treat some people with high cholesterol.
“The exciting part is these drugs have been [FDA] approved since 2015 and have been used by thousands of patients around the world,” said lead investigator Chuan-Yuan Li, D.Sc., of Duke University Medical Center. “They’re generally pretty safe,” Dr. Li said.
There may be other advantages, too, including that patients can take the medicines at home. The drugs are also less expensive than most cancer treatments, noted James Gulley, M.D., Ph.D., head of the immunotherapy group in NCI’s Center for Cancer Research.
“It opens up the possibility of doing a study to look at this combination” in people with cancer, Dr. Gulley added. Dr. Li and his colleagues are hoping to get a clinical study of the drug combination off the ground.
Both evolocumab and alirocumab block the activity of PCSK9, an enzyme that controls levels of “bad” cholesterol, also called LDL cholesterol. But the researchers found that the drugs’ effects on tumors had nothing to do with cholesterol. Instead, blocking PCSK9 made cancer cells more visible to cancer-fighting immune cells. Findings from the NCI-funded study were published November 11 in Nature.
The researchers are still exploring PCSK9’s role in cancer. The protein has multiple functions in healthy cells, Dr. Li said, so it may have other roles in cancer cells, too.
“We think there’s more to the story,” he added. The team is now doing experiments to see what other gene and protein changes occur in cancer cells lacking PCSK9.
Without PCSK9, Tumors Grow Slower
Dr. Li’s team stumbled into PCSK9 by chance. They had come across a study linking the activity of cancer-killing immune cells to an enzyme that regulates cholesterol.
“We thought, maybe we can investigate other cholesterol-regulating enzymes,” Dr. Li recalled. Around the same time, he learned that people who are born without PCSK9 have very low cholesterol levels and are protected from heart disease.
So, the team decided to look into whether PCSK9 plays a role in cancer. In lab experiments, cancer cells engineered to lack PCSK9 (by deleting the gene for the enzyme) grew at the same rate as cancer cells with PCSK9, the researchers found.
But when these cells were implanted into mice, they grew much slower than cancer cells with PCSK9. In addition, the PCSK9 inhibitors evolocumab and alirocumab both slowed the growth of colon tumors in mice.
PCSK9 affects blood cholesterol levels by controlling how much cholesterol receptor—a claw-like protein that grabs onto cholesterol and brings it inside—sits on the surface of liver cells. Blocking PCSK9 leads to more cholesterol receptors on cell surfaces and, in turn, less cholesterol in the blood.
The team suspected that the cancer-slowing effects of deleting or blocking PCSK9 had something to do with cholesterol. But, to their surprise, that didn’t appear to be the case. When they deleted the gene for the cholesterol receptor in skin cancer cells, it didn’t slow their growth down at all—nothing like the effects of deleting the gene for PCSK9 in those same cells.
Improving the Effects of Immune Checkpoint Inhibitors
Although PCSK9 is best known for its influence on the cholesterol receptor, it also controls the levels of other receptors on cells, including some that are involved in immune responses.
In line with that, Dr. Li’s group found that putting PCSK9-deleted cancer cells into mice triggered an immune response that slowed tumor growth.
What’s more, boosting the immune system with an immune checkpoint inhibitor slowed the growth of PCSK9-deleted tumors even further. In some experiments, treatment with an immune checkpoint inhibitor almost completely stopped the growth of PCSK9-deleted tumors.
Likewise, the combination of evolocumab or alirocumab plus an immune checkpoint inhibitor slowed the growth of tumors with PCSK9 more than any of the drugs alone. Mice treated with the combination also lived longer.
Helping the Immune System See Cancer
Next, the researchers explored how the immune system interacts with tumors lacking PCSK9. Given the enzyme’s role in regulating cell surface receptors, they focused there.
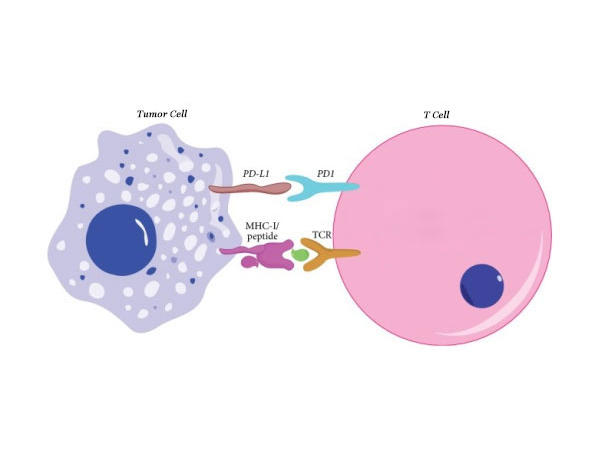
Before immune cells can kill cancer cells, they first have to find them. They do so by scanning the cell surface for MHC I, a protein that essentially shows what’s happening inside that cell. For cancer cells, MHC proteins often show that the cells are abnormal and should be removed.
“The only way a T cell can see what’s going on in a tumor cell is through the MHC molecule. It’s absolutely critical,” Dr. Gulley explained.
The researchers found that PCSK9 affects how much MHC I sits on the surface of cancer cells. Deleting PCSK9 or blocking its activity with evolocumab substantially raised the amount of MHC I on the surfaces of skin and breast cancer cells. In addition, PCSK9-deleted tumors contained more cancer-killing immune cells, including T cells, than tumors with PCSK9.
“If more [MHC] is around, T cells can interrogate more clearly what’s going on in the tumor. And immunotherapy is going to work better because the immune system can function better,” Dr. Gulley said.
On the other side of the coin, research has shown that immunotherapy doesn’t work well against tumors with mutations in MHC genes or other genes that help T cells see cancer cells. Other scientists are working on strategies to increase MHC levels in tumors, such as with radiation or immune-signaling molecules called cytokines, noted Dr. Gulley.