Temozolomide, a chemotherapy drug discovered and developed by our scientists, changed brain tumour treatment forever.
That’s not overselling it. Temozolomide was the first drug to improve survival for people with the most common and aggressive type of adult brain tumour: glioblastoma.
Professor Malcolm Stevens and his research team at Aston University set off on the journey that led to temozolomide back in the 1970s. In 1997, clinical trial results showed that it helped people with glioblastoma live longer and stay healthier. Combined with radiotherapy, it’s now the international standard of care for the disease.
More than that, though, temozolomide showed the world that there was a way forward against glioblastoma. It made what was beginning to look impossible possible, and it gave researchers hope.
“For a long time, there was a real feeling of utter nihilism, because nothing was working,” says Professor Anthony Chalmers from the University of Glasgow. “That put doctors and scientists off wanting to work in the area, and it put drug companies off wanting to invest. But temozolomide really changed that landscape, because, for the first time, some people clearly did respond to a drug.”
It was people like you – our supporters – who powered that change.
Chalmers is a doctor and a researcher who specialises in brain tumour treatment. Temozolomide is almost part of his job description. With our funding, he and his team are combining it with other drugs to make it more effective for people with glioblastoma.
But those aren’t just any other drugs. We’ve got plenty more milestones to go along with temozolomide. Chalmers’ team are bringing it together with another revolutionary medicine discovered and developed thanks to our funding and your support.
As we finish celebrating our 20th anniversary year, we want to focus on how they’re doing it. In many ways, the story of Chalmers’ new treatment technique is also the story of Cancer Research UK.
From BRCA genes to brain tumours
So, let’s go back to 2002. That’s when the Cancer Research Campaign (which supported the early development of temozolomide) and the Imperial Cancer Research Fund came together to form the world’s biggest independent cancer research charity: Cancer Research UK.
It didn’t take long to show what we could achieve. Just a year later, we funded the first clinical trial for a new class of drugs called PARP inhibitors.
These targeted treatments stop cancer cells repairing their DNA when it gets damaged. They do that by blocking the PARP (poly adenosine diphosphate-ribose polymerase) protein.
Today, doctors use PARP inhibitors to treat cancers caused by inherited defects or mutations in BRCA genes. That’s because, as well as raising some people’s risk of cancer, BRCA defects also make it harder for cancer cells to repair themselves. When they’re treated with PARP inhibitors, cancer cells with BRCA mutations have very few ways to repair their DNA. The damage builds up until the cells die.
BRCA stands for breast cancer, and BRCA defects are also linked to cancers that start from similar cell types, like ovarian and prostate cancer. Unhelpfully, though, brain tumour cells are completely different. PARP inhibitors can’t kill them.
Not on their own, at least. But treatments can team up, too.
“My research is really aimed at trying to get our standard care for glioblastoma working more effectively,” explains Chalmers. “And what radiotherapy and temozolomide have in common is that they kill the tumour cells by damaging their DNA.”
To a researcher like Chalmers, that looks like an opportunity.
“In that setting, you don’t need to have the BRCA defect for PARP inhibitors to do their job. The other treatments are inducing very high levels of DNA damage. The PARP inhibitors stop that damage being repaired and increase cell death.”
Crossing the blood-brain barrier
Chalmers makes that sound a lot easier than it actually is. Cancer drugs work by travelling through the bloodstream, but blood can’t carry things into the brain as easily as other organs.
 100vw, 150px”></p>
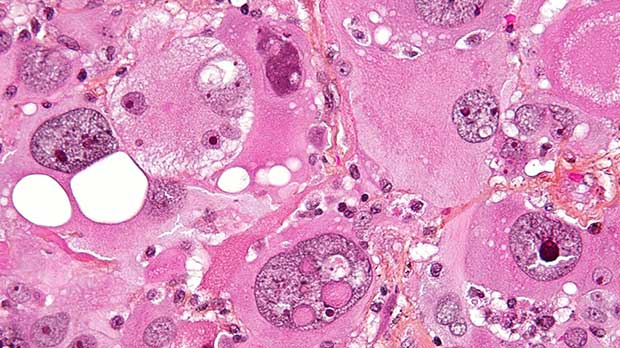
<p class=) There’s an especially strong barrier around blood vessels in the brain. ©2010 Ben Brahim Mohammed. CC BY 3.0
There’s an especially strong barrier around blood vessels in the brain. ©2010 Ben Brahim Mohammed. CC BY 3.0
This is because of a special system of brain cells called the blood-brain barrier (BBB). It’s there to stop potentially harmful substances getting in and causing life-threatening problems. You could compare to the skull, keeping the brain separate from its surroundings. This shield just protects against toxic chemicals rather than physical impacts.
Unfortunately, the BBB is also very good at keeping out cancer drugs.
One of the reasons temozolomide was such a breakthrough for brain tumour treatment is because it can pass through the BBB. In 2011, Chalmers launched a trial called OPARATIC to find out if the PARP inhibitor olaparib could, too.
Before the team started their work, the signs didn’t look good. Olaparib is mainly used to treat ovarian cancer. We funded its developers, but they weren’t thinking about getting it into the brain.
Surprisingly, though, it turned out that glioblastomas actually disrupt the BBB just enough to let olaparib through. From there, it can make the tumours more sensitive to temozolomide and radiotherapy.
“What’s exciting about this is that the PARP inhibitors increase the effectiveness of both radiotherapy and temozolomide,” Chalmers says. “So we’re hopeful that if we give all three together, we’ll have a really powerful effect on the tumour.”
That’s what they’re testing now.
Treating brain tumours with PARP inhibitors
Since OPARATIC, Chalmers and his team have launched 2 more clinical trials testing combinations of olaparib, temozolomide and radiotherapy as treatments for people with newly diagnosed glioblastomas.
They’re called PARADIGM and PARADIGM-2, and both are currently in phase 1, the stage when doctors work out the highest safe dose they can give to patients. PARADIGM is for patients over 65, while PARADIGM-2 can include anyone under 70.
In both trials, patients are sorted into different groups depending on how likely they are to benefit from temozolomide. That depends on whether their tumours suppress the production of a protein called MGMT, which can repair the DNA damage caused by the drug.
MGMT is only suppressed (or methylated) in around half of people with glioblastomas. Olaparib could be the first effective brain tumour treatment drug for people with unmethylated MGMT. And, while olaparib and temozolomide look like a potent combination for the other group, giving people both also raises the risk of side effects, so the doses need to be worked out very carefully.
“In both of those groups of patients, we are now getting close to what we think will be the final dose that we can give,” says Chalmers. “It also looks like the patients are doing quite well in terms of survival. We don’t have the definitive data, but what we’re seeing is encouraging.”
The future of brain tumour treatment
As the PARADIGM trials continue into their later phases, we’ll begin to see that definitive data about how adding olaparib can improve how we treat glioblastoma. The signs so far are especially welcome: brain tumours are one of the most difficult challenges in cancer research. Advances like temozolomide have helped double brain tumour survival over the past 40 years, but it’s still lower than almost any other cancer type.
That’s why we highlighted brain tumours as a “cancer of unmet need” in 2014. Since then, we’ve doubled our funding in the area and built the kind of collaborations – between charities, universities, pharmaceutical companies and research institutes – that we know are necessary to speed up progress. It’s all designed so we can tackle the unique challenges presented by cancers in the brain.
“It’s a very, very specific environment,” stresses Chalmers. There’s the blood-brain barrier, for a start, and then there’s the difficulty of killing cancer cells without damaging the healthy ones around them – the ones we think, act, share and learn with; that make any of this possible.
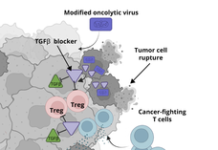
“And the immune system is completely different in the brain than it is in the rest of the body,” Chalmers adds. “We now know that we can get much better responses to therapy if we can engage the immune system to attack tumours as well. But that doesn’t seem to happen in the brain.”
Solving those problems takes expertise and commitment. If it wasn’t for temozolomide, there might not be so much of that available.
Chalmers and his fellow researchers are showing how our legacy of funding lifesaving research powers the advances we’re aiming to make in the future. We’re behind them, and many others like them, all the way.
Tim

 ©2011
©2011