, by NCI Staff
Both the number of cases of anal cancer and deaths from the disease have been on the rise in the United States since 2001, according to a new study. The increases have been especially rapid in young African American men, as well as among all adults over the age of 50.
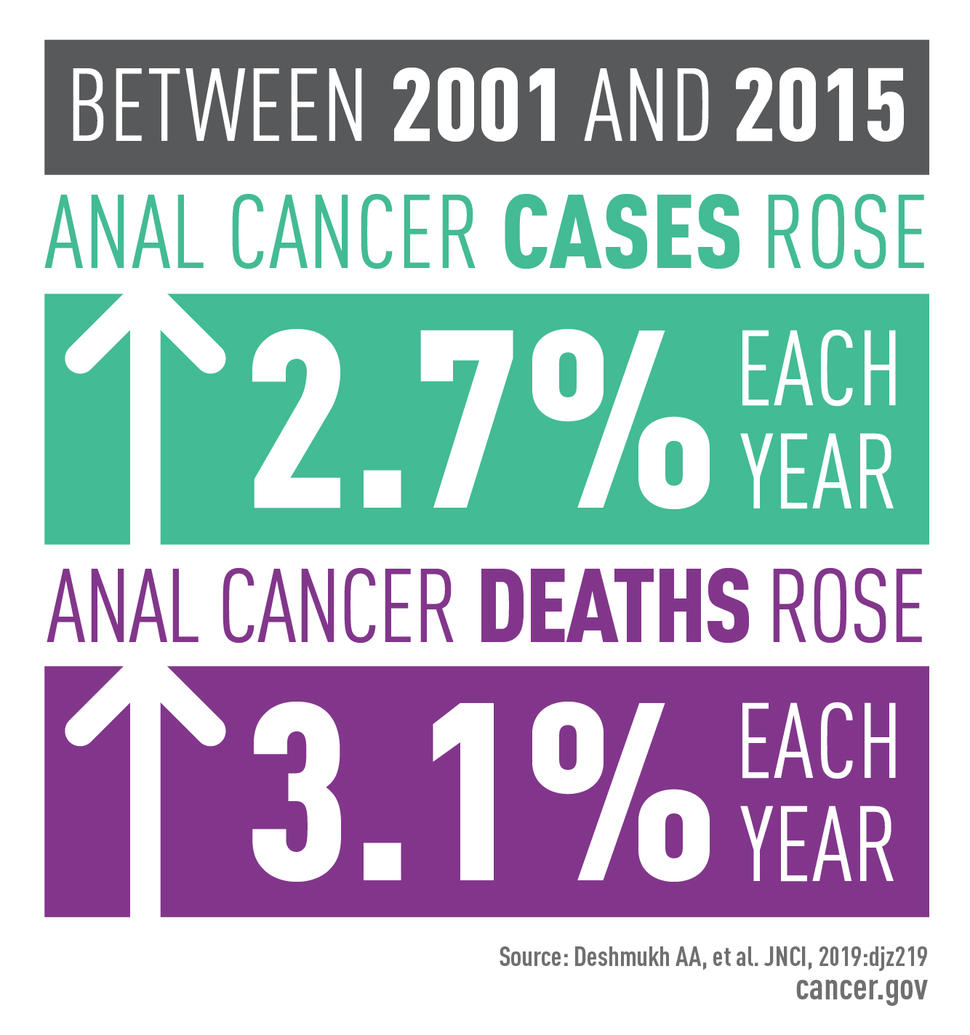
From 2001 to 2015, the overall incidence of anal cancer increased by 2.7% per year and mortality jumped by 3.1% each year, according to the study, published November 19 in the Journal of the National Cancer Institute.
Despite these increases, anal cancer is “still quite rare in the population,” explained Meredith Shiels, Ph.D., of NCI’s Division of Cancer Epidemiology and Genetics (DCEG), a coauthor on the study.
Most cases of anal cancer are caused by infection with human papillomavirus (HPV). A vaccine to prevent HPV infection has been available since 2006, but the cancers seen in this study reflect HPV infections acquired before the vaccine was available.
Higher vaccine uptake than has been achieved to date is needed to reverse the rise of anal cancer incidence and mortality, said Ashish Deshmukh, Ph.D., M.P.H., of the UTHealth School of Public Health in Houston, who led the study.
Trends in a Rare Cancer
To understand trends in anal cancer over the last few decades, Dr. Deshmukh and his colleagues used data on cancer incidence collected by NCI’s Surveillance, Epidemiology, and End Results (SEER) program and the CDC’s National Program of Cancer Registries (NPCR).
Cancer death data for the corresponding period came from the National Center for Health Statistics. The researchers also looked at changes in incidence over time among groups defined by sex, race, age, and year of birth.
Between 2001 and 2015, they found, almost 70,000 people in the United States received a diagnosis of anal cancer. The majority were female, white, and over the age of 50. But some groups had an even greater increase in risk. For example, adjusting for age, the risk of anal cancer among young African American men born around the mid-1980s was five times higher than that in African American men born in the late 1940s.
“This finding was particularly sobering, because these men are very young” compared with the age range of people typically diagnosed with anal cancer, said Dr. Deshmukh. This high incidence, he said, is likely driven by the higher rate of human immunodeficiency virus (HIV) infection among younger black men in the United States. HIV weakens the body’s ability to fight off HPV infection.
In addition to the overall rising incidence, the number of cases of anal cancer diagnosed at a later stage—when the cancer had already spread to nearby or distant parts of the body—also increased between 2001 and 2015. During this time period, diagnoses involving advanced disease tripled in men and more than doubled in women.
These rising rates of advanced-stage disease likely underly the increases seen in deaths from the disease, particularly in older adults, noted the authors. For example, they saw a nearly 5% increase in deaths from anal cancer per year in people aged 60 to 69.
A Viral Trigger
HPV is a group of more than 200 related viruses, some of which are spread through vaginal, anal, or oral sex. Most of these viruses do not cause cancer. But about 14 sexually transmitted HPV types are known to cause six types of cancer: cervical cancer, oropharyngeal (throat) cancer, and anal, penile, vaginal, and vulvar cancers.
Two types, HPV16 and HPV18, are responsible for most HPV-caused cancers. Even if someone is infected with one of these viruses, though, the immune system can usually eliminate the infection. But in some people, the infection persists, and infected cells eventually become cancerous. This risk that an infection will persist is higher in people with weaker immune systems, including older adults and people living with HIV.
It takes about two decades or more for HPV infection to lead to cancer, explained Dr. Deshmukh. This means that cases of anal cancer observed in the study would be related to HPV infections contracted in the 1990s or earlier, before a vaccine to prevent infection with cancer-causing HPV types was available.
Screening and treatment of precancerous changes in the cervix caused by HPV have reduced the incidence of cervical cancer in women aged 50 and older by 65% since the 1970s. But to date, no screening method has been shown to reduce the risk of anal cancer, said Dr. Shiels.
The rising incidence of anal cancer has been on researchers’ radars for some time, even if the extent of the increase wasn’t highlighted until now. Some efforts have already begun to test screening strategies for some of the populations at highest risk, Dr. Shiels said.
For example, an NCI-funded clinical trial called ANCHOR is currently testing whether treatment of precancerous anal lesions can prevent the development of anal cancer in men and women with HIV.
Even with the rising incidence over the last two decades, “only about 8,000 cases of anal cancer are diagnosed in the United States each year,” said Dr. Shiels. “Examining screening in this highest-risk population makes sense at this time.”
Hard Conversations
In the absence of evidence of effective screening tests, like the Pap and HPV tests for cervical cancer, to prevent the incidence of anal cancer from continuing to rise in the future, “emphasis should be on rapidly scaling up HPV vaccination rates,” said Dr. Deshmukh.
Many barriers have kept US HPV vaccination rates around 50% in the recommended age groups, with significant variation between states. One barrier is that many people still don’t know that HPV causes cancer. In a study published earlier this year, Dr. Deshmukh and his colleagues found that fewer than 30% of adults surveyed knew that HPV could cause anal, oral, and penile cancers. And a substantial number of young adults didn’t even know that the virus causes cervical cancer.
To improve HPV vaccination rates, better communication between health care professionals, people eligible for the vaccine, and their families is crucial, said Dr. Deshmukh. Those discussions should be driven by the CDC’s most recent recommendations on HPV vaccination.
But in the earlier study conducted by Dr. Deshmukh and his team, only about 20% of vaccine-eligible men and about 30% of vaccine-eligible women or people with vaccine-eligible family members had ever received a recommendation for HPV vaccination from their doctor. Overcoming physicians’ reluctance to recommend the HPV vaccine “has great potential” to improve its use, he said.
There is also a need for more awareness and less stigma around anal cancer, explained Haisar E. Dao, M.D., of the University of Texas Health Science Center at San Antonio, who was not involved with the study.
“People think that anal cancer only occurs in people who are immunosuppressed, or have HIV, or who are men who have sex with men,” Dr. Dao said. “And although these populations are more at risk of anal cancer, it’s not exclusive to these population.”
Symptoms of anal cancer can include bleeding, pain in the anal region, and swelling or lumps in the area. “Anyone with symptoms should be seen by a specialist as soon as possible,” he added.
Such conversations require overcoming taboo and embarrassment, Dr. Dao explained. “People don’t want to talk about any anal or rectal conditions. But it’s important not to minimize any [of these] symptoms.”
People often think that these symptoms must be caused by hemorrhoids and can be ignored, added Dr. Dao. And while that’s a likely explanation, “a few times we’ve found very advanced cancers that could have been caught earlier,” he said.
And earlier diagnosis can be important, Dr. Deshmukh stressed. “[Mortality] can often be avoided if we diagnose anal cancer early.”