Leicester Royal Infirmary EM Department
Leicester Royal Infirmary EM Department
Sacituzumab govitecan (Trodelvy) is not being recommended by the National Institute for Health and Care Excellence (NICE) for use in England as a treatment for some people with triple-negative breast cancer (TNBC).
Clinical trials reveal that the targeted treatment is proven to help treat aggressive TNBC in patients who have already had two previous therapies. However, the drug is not currently considered a cost-effective treatment for NHS England, according to NICE draft guidance.
This decision will be disappointing for people affected by triple-negative breast cancer that’s spread locally or to other parts of the body, as there are currently very limited effective treatment options for these patients.
Rose Gray, head of policy development at Cancer Research UK.
An aggressive breast cancer
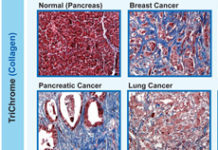
There are an estimated 2,000 people living with TNBC in England. However, despite only accounting for 15% of all breast cancer cases, TNBC is responsible for a quarter of all deaths from breast cancer in England, making it a particularly aggressive form of the disease.
TNBC does not have any of the three molecular markers (oestrogen, progesterone and HER2 receptors) commonly found in other types of breast cancer. Because TNBC is not sensitive to hormone therapy or molecular targeted therapy, this significantly reduced treatment options and prognosis for patients, with chemotherapy being the main form of treatment.
New targeted treatment
Sacituzumab govitecan could provide a new treatment option for people with TNBC who have already had two or more prior systemic therapies.
The drug works by targeting the activity of Trop-2 proteins that are present at high levels on the surface of tumour cells. It then delivers the anti-cancer component of the drug directly to tumour cells, preventing the cells from multiplying and eventually causing them to die.
A randomised open label clinical trial involving 468 eligible patients confirmed that people treated with sacituzumab govitecan had a longer period of time before their cancer grew compared to the physician’s chemotherapy of choice. Those given sacituzumab govitecan lived for an average of 11.8 months, compared to 6.9 months in the treatment of physician’s choice arm.
Additionally, the percentage of patients whose tumours shrunk was greater in the group who received sacituzumab govitecan at 31.1%, compared with 4.2% in the treatment of physician’s choice arm.
Of the 2,000 people in England with TNBC, around 650 would have been eligible for treatment with sacituzumab govitecan if the drug was recommended by NICE.
NICE say no to sacituzumab govitecan
Despite its effectiveness, draft guidance by NICE does not recommended sacituzumab govitecan for use on NHS England due to its high cost. An alternative treatment recommended by NICE is a type of immunotherapy known as atezolizumab (Tecentriq) in combination with chemotherapy.
“Because sacituzumab govitecan is a highly effective treatment, and given the lack of treatment options for people with this type of breast cancer, we’re very disappointed that its price means we can’t recommend it for use in the NHS at this point.
“We hope that the company will consider what it can do to enable NICE to approve a treatment that has the potential to give people with advanced triple negative breast cancer more time with their loved ones,” says Helen Knight, interim director of medicines evaluation at NICE.
“We recognise that the time and cost it takes to develop a new medicine means cancer drugs can often come with high price tags and we urge the NHS and drug companies to consider long-term solutions to this. Drug prices should ensure value for money for the NHS while also rewarding companies for innovative treatments that benefit cancer patients,” adds Gray.
The draft guidance is available for public consultation until 29 April 2022. A final decision is expected to be made by June 2022.
NICE decisions are usually adopted in Wales and Northern Ireland as well as England, so the decision is likely to affect patients in all 3 nations, however the drug was approved by the Scottish Medicines Consortium (SMC) for use in Scotland last month.